We know about rehabilitation, but have you heard of prehabilitation? It’s the practice of preparing patients for an upcoming surgery with healthy lifestyle behavior practices. Researchers say the benefits are worth the effort.
In the weeks before the surgery, prehabilitation encourages patients to move more, eat healthier, cut back on tobacco, breathe deeper, reduce their stress and focus on their goals after their operation.

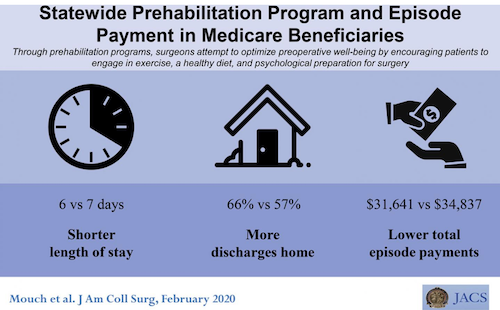
A University of Michigan study looked at the practice used across 21 hospitals statewide and found that this inexpensive program helps patients physically and mentally prepare for surgery. On the other side of surgery, prehabilitation reduced the length of hospital stays, increased the number of discharges directly to one’s home and not surprisingly, it lowered costs.
In as early as 2017, University of Michigan tested the idea and found the approach reduced total medical costs related to the patient’s care and cut their length of stay in the hospital, compared with similar Michigan Medicine patients who had surgery before the program began.
This new study expanded the program across the state on a more rigorous scale. The results, published in the Journal of the American College of Surgeons, used data from 523 patients with traditional Medicare coverage who went through “prehab”, and more than 1,000 similar patients who did not.
Prehab patients across the state left the hospital one day earlier, and were more likely to go straight home rather than to a skilled nursing facility, compared with similar patients treated at the same hospital. Total costs for all care up to three months after surgery were nearly $3,200 less on average for those who went through prehab.
Prehabilitation practices by operating room teams
For a second new study published in Annals of Surgery, the researchers proposed that surgical teams adopt the same “positive psychology” approach to engaging with surgery candidates that patients in the study were taught.
“Every time the prehab study has been studied, it’s found to increase the value of surgical care by improving care while reducing cost. This study cements the business case for hospitals to support it,” says Michael Englesbe, M.D., who leads the U-M Department of Surgery team that has published both studies and others.
“We also now recognize that prehab’s physical training may work partly because it empowers the patient to engage in their own recovery,” adds Dr. Englesbe, a professor of surgery and director of the Michigan Surgical Quality Collaborative. “Patient empowerment is the ‘secret sauce’ and we hope to harness it even more.”
Low-cost intervention for high-risk patients
The new study focused on the patients with the highest risk of complications after surgery because they had a combination of underlying health conditions beyond the problem that required surgery. Their median age was 70, and one-in-six qualified for federal disability benefits. All of them, and the patients they were compared with, were having one of 26 common operations.
The prehab patients’ surgeons referred them to the program, called the Michigan Surgical and Health Optimization Program or MSHOP. The program was supported by a grant from the Center for Medicare and Medicaid Services, and involved hospitals taking part in the MSQC quality improvement program.
- Once enrolled, they received a call or electronic message from a member of the MSHOP team, and materials about the importance of better nutrition, tobacco cessation, engaging in positive thinking and goal-setting, and reducing stress to their pre-surgery preparation.
- They also received a pedometer to track their steps, and an incentive spirometer to encourage them to practice taking deep breaths, to improve their lung function before and after surgery.
- In all, 62% of them tracked their walking three or more times a week, entering them into their medical record or calling them in to a secure voicemail box. The program staff contacted patients who hadn’t logged steps, to encourage them to do so. For those who tracked regularly, they took an average of 2,909 steps per day, and about 30 deep breaths on the spirometer.
The comparison group of patients was chosen to match the type of operation, and the hospital where they had surgery. Though the prehab patients were only in the program for an average of two and a half weeks before surgery, the program was associated with statistically significant changes in several measures.
In addition to the total cost and hospital length of stay differences, the patients in the program were less likely to need home health care after they went home, with 24% of the prehab patients receiving it compared with 29% of non-prehab patients. However, the prehab patients had about the same rates of nursing home stays, visits to emergency departments and additional hospital stays after they left the hospital.
Next steps in prehabilitation
Although prehab programs at many of the participating hospitals ended or scaled back when the study ended, the U-M team has made MSHOP part of the standard of care for Michigan Medicine surgical candidates who have a higher than usual risk of complications. Blue Cross Blue Shield of Michigan supports the effort through a pilot payment project. A full kit of patient materials is available online.
In addition to incorporating more positive psychology aspects, such as having patients express their post-surgical goals and the steps they will take to try to reach them, the MSHOP program has evolved to allow patients to track steps using their smartphones and wearable activity trackers instead of providing pedometers. The program has even been integrated into the electronic portal that patients use, so that they can sync their step counts automatically from their device. Surgical team members, from pre-op clinic staff to post-surgery rounding teams, are encouraged to work with MSHOP enrollees toward shared ownership of their surgical outcomes, and better wellbeing.
Dr. Englesbe says this can work in any setting. He encourages practitioners to help anyone getting ready to have surgery to try to increase their physical activity, improve their nutrition, reduce or eliminate tobacco use and focus on their mental state.
For instance, patients should be encouraged to actually write down their own goals for life after surgery – what activities they hope the operation will allow them to do again or more fully, or life events they are looking forward to. They can also write down the specific steps they will pledge to take to help them attain this – for instance, a physical activity goal or new nutritional habit. Another great step is to write down the names of their family and friends who will support them before and after surgery, and their roles, and to share this with the care team.
If information like patient goals and support people makes it into the patient’s medical record, members of the care team can use it too. For instance, they can use the “time out” that precedes the start of every operation to review not only what operation they’re doing, but the goals of the patient having it. Or they can use it when doing rounds in the hospital, to prepare them to have a more engaging conversation with the patient. As they write in the paper, teams should remember that they’re not just doing surgery to solve the patient’s physical problem, but to help the person who has the problem.
Conclusion/ Participation in a prehabilitation program in Michigan was associated with shorter length of stay and lower total episode payments after operation. Researchers encourage payers, hospital and practitioners to invest in the implementation of simple home-based prehabilitation programs.
Click Here for Full Text Study