Over the last decade or so, research interest in the pro-inflammatory and pro-fibrotic immune protein galectin-3 (Gal-3) has skyrocketed. Today, thousands of published scientific papers—including longitudinal cohort studies—point to the driving role of galectin-3 in the pathogenesis of our most serious degenerative conditions, from chronic kidney disease and acute kidney injury to cardiovascular disease, Alzheimer’s, Parkinson’s, metastatic cancer, autoimmune disease, and many others.
Galectin-3 normally exists in the body at relatively low concentrations, where it plays fundamental roles in immune activity, normal growth and development, and inflammatory repair processes. Levels rise in response to various stressors and triggers, including psychological stress, infections, injury, and even normal aging. As a beta-galactoside binding protein that is at the headwaters of the body’s inflammatory cascade, galectin-3 is emerging as a key driver of chronic disease processes involving inflammation and fibrosis of organs and tissues. When galectin-3 is secreted into the extracellular space at a site of injury or inflammation, it activates resting fibroblasts which become matrix-producing fibroblasts that express pro-fibrotic proteins.
Galectin-3 is monomeric but can oligomerize into pentamers that bind to various ligands to form the backbone of fibrotic tissues, biofilms, atherosclerotic plaque and other hyperviscous structures. As research into its pathogenic mechanisms continues to expand, galectin-3 is increasingly recognized as a predictive biomarker and novel therapeutic target for a rising number of pro-inflammatory conditions, most notably cancer, heart failure and neurodegenerative disease.
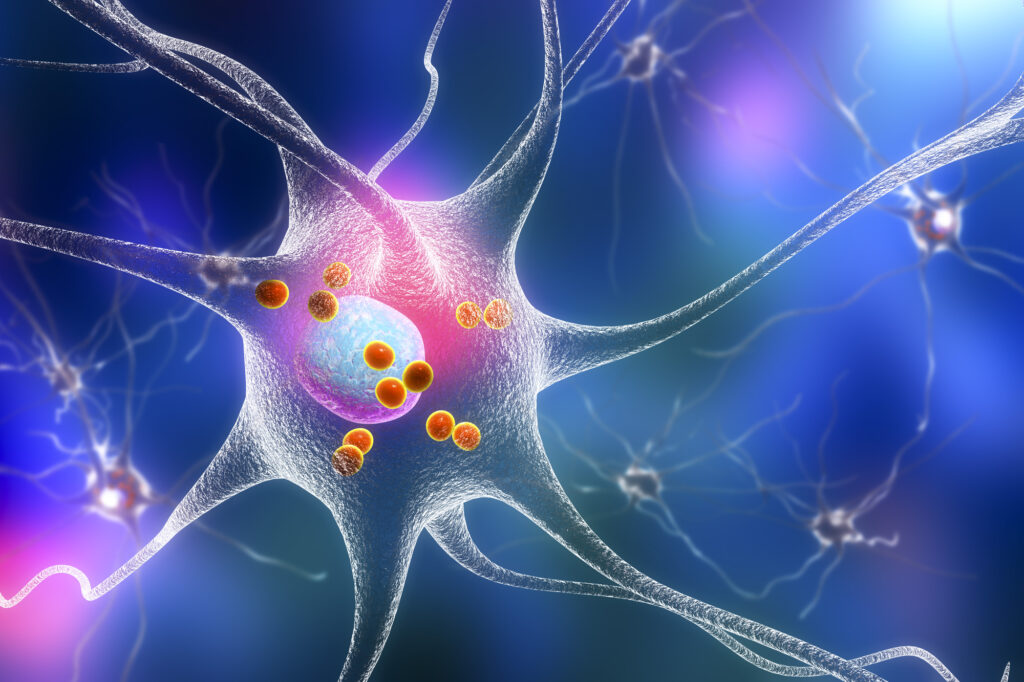
Galectin-3 and Neurodegeneration
In recent years, galectin-3 has emerged as a key driver of neuroinflammation and neurodegenerative disease. It modulates the immune response in the CNS and activates microglia to a proinflammatory state. Research also shows it plays a role in the aggregation of amyloid-beta peptides and can influence toxicity of amyloid-beta. It is also suggested to play a role in oxidative stress contributing to neuronal injury and death. Other data showed that galectin-3 levels in the brain were upregulated and linked to neuroinflammation in spinal cord injury and Huntington’s disease, through activation of the NLRP3 inflammasome pathway.1,2
Defending Against Ischemic Damage to the Brain
Stroke, specifically ischemic stroke where blood flow to the brain is blocked, is the second most common cause of death worldwide, and a significant cause of disability and loss of function. Swift, timely intervention immediately following a stroke event can support better clinical outcomes by mitigating damage to the brain and central nervous system (CNS); however, there is an urgent need for effective treatments that can reduce the devastating neurological impacts of common stroke events.
A growing body of data points to microglial neuroinflammation as a contributing factor in ischemic stroke injury — driven by high levels of galectin-3. Unregulated microglial activation (which can happen in response to toxins, stroke injury, illness, etc.) produces neurotoxic compounds that fuel neurodegeneration and neurological diseases.
Research shows that Gal-3 promotes unregulated microglial activation and proliferation during stroke, driving neuroinflammation and damage to the brain. A published study highlights this mechanism of Gal-3 in ischemic stroke injury, and shows how the researched nutraceutical, Modified Citrus Pectin (MCP), blocks the proinflammatory actions of Gal-3 in ischemic stroke, to provide significant neuroprotection for the brain.
The study, published in the Journal of Inflammation Research, shows how MCP reduced neurological deficit, brain water content, and infarction volume, as well as relieved cell injury in the cerebral cortex. MCP was also shown to increase cell viability and reduce cell apoptosis, while blocking galectin-3 and decreasing the expression of proinflammatory factors such as NF-kB and TLR4 in microglial cells.3
This new study demonstrates the neuroprotective benefits of MCP, building on data from previous research showing how MCP helps prevent cognitive decline and defends against Alzheimer’s disease.
Galectin-3, Alzheimer’s, and Cognitive Decline
A study in the Journal of Diabetes Investigation showed how Gal-3 acts as a driving factor in the development of diabetes-related cognitive loss and Alzheimer’s disease. This study highlighted the role of Gal-3 as a key driver of metabolic dysfunction and cognitive decline.4
The study showed for the first time that MCP prevents cognitive impairment in a diabetes animal model. The MCP-treated group showed significant improvements in learning and memory, compared to controls.
Another study from 2020, published in the Journal of Inflammation Research, further elucidates these mechanisms and confirms that the researched form of MCP is effective in blocking Galectin-3 in the brain and protecting against neuroinflammation and cognitive decline.5
Data from this study highlights several key protective benefits offered by MCP for neurological health: MCP reduced cognitive impairment, insulin resistance, oxidative stress and neuroinflammation. Results also demonstrated that MCP improved oxidative stress and the inflammatory response.
These findings are significant because they further demonstrate Gal-3 as a therapeutic target in the management of neurological health and cognitive disease. They also add to the list of essential benefits offered by the researched form of MCP— most researched Gal-3 blocker available today — as a powerful therapeutic adjunct for the spectrum of degenerative diseases fueled by upstream inflammation driver, Gal-3.
RELATED:
Blocking Galectin-3 with Modified Citrus Pectin
Author Bio:
Dr. Joshua Helman, MD is a Harvard-trained physician licensed in 14 states. He holds two degrees in biochemistry, a bachelor’s degree (magna cum laude) from Harvard and a master’s degree from the University of Cambridge, UK. His medical degree is from Harvard Medical School and MIT. He is board certified by the American Board of Emergency Medicine and the American Board of Lifestyle Medicine. He is the former medical director of Hippocrates Health Institute and has worked at the TrueNorth Health Center with a focus on fasting.
Dr. Helman, a plant-based physician, has dedicated six years to reversing and preventing Alzheimer’s disease in patients. His areas of interest span longevity, regeneration, vitality, toxins, mold, Lyme disease, energy medicine and breathwork. With a passion for applying biochemical knowledge to real-world challenges, he embraces a holistic approach that emphasizes the importance of diet and lifestyle for optimal health.
Dr. Helman is inspired by people’s ability to change their bad habits and adopt a better lifestyle, in order to prevent, improve and reverse chronic diseases like Alzheimer’s.
References:
- Zhouliang Ren, Weidong Liang, Jun Sheng, Chuanhui Xun, Tao Xu, Rui Cao, Weibin Sheng; Gal-3 is a potential biomarker for spinal cord injury and Gal-3 deficiency attenuates neuroinflammation through ROS/TXNIP/NLRP3 signaling pathway. Biosci Rep.20 December 2019; 39 (12): BSR20192368.
- Siew JJ, Chen HM, Chen HY, Chen HL, Chen CM, Soong BW, Wu YR, Chang CP, Chan YC, Lin CH, Liu FT, Chern Y. Galectin-3 is required for the microglia-mediated brain inflammation in a model of Huntington’s disease. Nat Commun. 2019 Aug 2;10(1):3473.
- Cui Y, Zhang NN, Wang D, Meng WH, Chen HS. Modified Citrus Pectin Alleviates Cerebral Ischemia/Reperfusion Injury by Inhibiting NLRP3 Inflammasome Activation via TLR4/NF-ĸB Signaling Pathway in Microglia. J Inflamm Res. 2022 Jun 9;15:3369-3385.
- Ma S, Li S, Lv R, Hou X, Nie S, Yin Q. Prevalence of mild cognitive impairment in type 2 diabetes mellitus is associated with serum galectin-3 level. J Diabetes Investig. 2020 Sep;11(5):1295-1302.
- Yin Q, Chen J, Ma S, et al. Pharmacological Inhibition of Galectin-3 Ameliorates Diabetes-Associated Cognitive Impairment, Oxidative Stress and Neuroinflammation in vivo and in vitro. J Inflamm Res. 2020;13:533-542.