A histamine intolerance is thought to trigger a plethora of clinical symptoms after ingesting histamine‐rich foods that may be linked to the reduced activity of an enzyme, diamine oxidase (DAO), an enzyme responsible for clearing the body of histamines. No study to date has systematically assessed daily fluctuations of histamine levels and DAO activities in symptomatic patients. This study, published in Allergy, European Journal of Clinical Immunology, aimed to investigate the presence of histamine intolerance, establish day profiles of histamine levels and DAO activities, and to compare the results between patients with suspected histamine intolerance, food allergy and healthy controls. Link to full text available at the end of the study.
Histamine intolerance is a confusing disorder for both the patient and practitioner. Studies show that it is a causal trigger for a number of gastrointestinal disorders, such as abdominal pain, diarrhea and flatulence. The symptoms frequently resemble irritable bowel syndrome (IBS). However, other symptoms fall outside the IBS scenario, such as headaches, pruritus, urticaria, atopic eczema, cardiac arrhythmia and asthma. Finding a solution is extremely difficult and frequently lies with the patients using a trial and error histamine intolerance diet (know as HIT).
As both the aetiology and the course of histamine intolerance are not sufficiently investigated, the knowledge and treatment in the medical field are not always uniform. Thus, affected patients do doctor shopping to find an appropriate explanation for their diversified complaints.
The frequency of histamine intolerance is not fully understood yet, but early evidence suggests that about 1%‐3% people are affected, mostly mid-age women. The hypothesis is that reduced activity of diamine oxidase (DAO), the key enzyme in histamine metabolism, is the main factor in the development of histamine intolerance. When DAO activity is low, this leads to an accumulation of histamine above the individual critical value. Oddly, this may provoke symptoms of the disorder within an hour or even days of consuming the offending food. Reduced DAO is not the only causal factor, ingesting histamine‐rich and histamine‐releasing foods such as meat, dairy products and alcohol may also incite reactions. Seemingly healthy foods such as yogurt, spinach, tomatoes, nuts, wine vinegars and beans may cause reactions among histamine intolerant individuals.
key enzyme in histamine metabolism, is the main factor in the development of histamine intolerance. When DAO activity is low, this leads to an accumulation of histamine above the individual critical value. Oddly, this may provoke symptoms of the disorder within an hour or even days of consuming the offending food. Reduced DAO is not the only causal factor, ingesting histamine‐rich and histamine‐releasing foods such as meat, dairy products and alcohol may also incite reactions. Seemingly healthy foods such as yogurt, spinach, tomatoes, nuts, wine vinegars and beans may cause reactions among histamine intolerant individuals.
In this study, researchers determined the day profiles of histamine plasma levels and DAO serum activities in 33 patients with suspected histamine intolerance, in 21 patients with proven food allergy and in 10 healthy control patients. Clinical symptoms, food intolerances and further clinical and laboratory chemical parameters were evaluated.
This study is unique in that so far, “no study has systematically assessed daily fluctuations of histamine levels and DAO activities in symptomatic patients.”
Study Parameters
Over a 12‐month period, a total of 65 adult patients were enrolled in the study. Twenty‐four percent (8 of 33) suspected histamine‐intolerant patients showed elevated histamine levels during the day. That might be caused by constantly and significantly reduced DAO activities in these patients compared to food‐allergic and control patients. The remaining 25 patients presented normal histamine levels and DAO activities, but an increased prevalence of multiple food intolerances compared to the other subgroup of suspected histamine‐intolerants. There was no correlation between subjective complaints and serological histamine parameters in patients with suspected histamine intolerance.
A 3‐day nutritional diary using the Freiburger Diet Protocol (Nutri‐Science GmbH, Freiburg, Germany) directly before the time of investigation was itemized in energy value as well as content of protein, fat, carbohydrates and alcohol per day by PRODI (version 6.5 expert, Nutri‐Science GmbH). All patients were checked for sugar intolerances in‐house or externally by validated H2 breath tests. The survey at the examination day assessed clinical symptoms, underlying diseases and both nicotine and alcohol consumption. Furthermore, IBS symptoms were recorded using questionnaires based on the Rome III criteria.
To determine a day profile of both histamine levels and DAO activities at the examination day, blood samples were taken every three hours from 6 am until midnight by butterfly needles or peripheral venous catheters.
Additional blood samples were taken for further investigation of a differential blood count (reference range neutrophil granulocytes <75%, eosinophil granulocytes <4%, basophil granulocytes <1%, lymphocytes <40% and monocytes <8%) and for vitamin B6 determination (reference range 5.0‐30.0 ng/mL).
Histamine Intolerance Testing Results
As expected, the IgE antibodies were significantly increased in the food‐allergic patients (361.2 ± 911.2 kUA/L) (P < .001), whereas the IgE antibodies were in the normal range in the suspected histamine‐intolerants (29 ± 24.4 kUA/L) and healthy volunteers (14.3 ± 9.6 kUA/L). Correspondingly, proven food‐allergic patients were tested positive for nut mixture (76.2%), wheat flour (47.6%), celery (42.9%), tomato (23.8%), rye flour (23.8%), soybean (14.3%) and milk protein (4.8%) and negative for chicken egg white, casein and salmon.
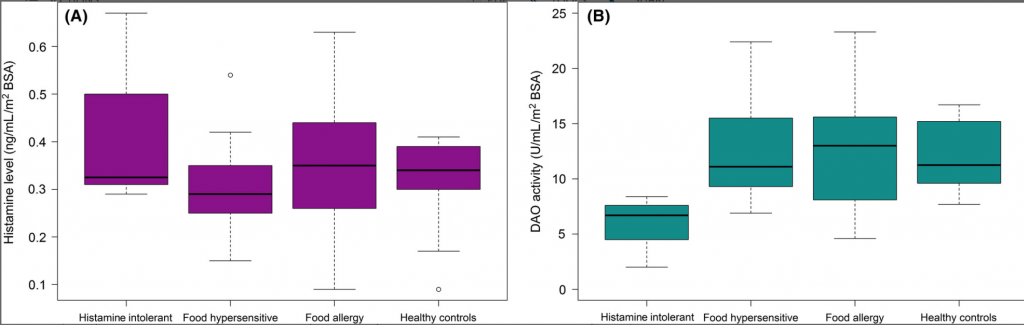
Diamine oxidase (DAO) activities were significantly lower in histamine‐intolerants (see Figure 2) and tended to be within the normal range in the other groups. There were no significant differences between the groups regarding the bandwidth of histamine levels (see Figure 2 below).
The overall prevalence of food intolerances in symptomatic patients did not differ significantly between groups. Splitting the food intolerances against fructose, lactose and sorbitol into single and multiple intolerances revealed an intriguing result: histamine intolerance was exclusively associated with single food intolerances, whereas food‐hypersensitive and food‐allergic patients showed similar percentages of single and multiple food intolerances.
In general, histamine‐intolerant, food‐hypersensitive and food‐allergic patients presented a wide variety of symptoms. No differences between these groups were seen in the prevalence of symptoms (see Table 2). Further self‐reported disorders, for example palpitations, flush, heartburn, nervousness, fatigue, increased sweating, muscle and joint pain, were infrequent (<15% each), except for flatulence (histamine‐intolerant patients: 12.5%; food‐hypersensitive patients: 25%; food‐allergic patients: 19%).
FIGURE 2
Conclusions
For the first time, we were able to demonstrate that there are patients who can be classified as histamine‐intolerants according to the definition. In 24% (8 of 33) suspected histamine‐intolerants, constantly and significantly reduced DAO activities triggered elevated histamine levels throughout the day. We observed that the most common clinical symptoms of histamine intolerance are diarrhea, nausea and vomiting, headache, itchy skin, oral allergy syndrome as well as red eyes and swollen eyelids (≥50%). These findings appear to be consistent with literature data as gastrointestinal, skin and respiratory problems as well as headache have been described to be characteristic for histamine intolerance.
We determined by daily profiling that decreased DAO activities correlated with elevated histamine levels in a subgroup of suspected histamine‐intolerants. This finding discriminates these patients from food intolerant individuals with similar clinical symptoms and strongly suggests the presence of histamine intolerance.





