A study in The Lancet shows that one-in-two hospitalized COVID-19 patients develop one-or-more complications. They include renal, complex respiratory, and systemic complications, as well as cardiovascular, neurological, and gastrointestinal and liver complications. Overall, complications occurred in 50% of all participants, including in 44% (21,784 of 50,105) of participants who survived.
The association between having a complication and worse ability for self-care remained irrespective of age, sex, socioeconomic status, and which hospital someone received treatment in. Neurological complications were associated with the biggest impact on ability for self-care.
Today’s Practitioner believes these results point to a greater need for naturopathic and integrative physicians to work in primary care and specialty clinics to better serve these patients and address the complexity of care that is required for them to re-enter society.
Complications Spread Across All Demographics
The complications were not limited to one age group. Men and those aged older than 60 years were most likely affected, but complications and poor functional outcomes were common, even in younger, previously healthy adults.
- 27% of 19-29 year olds and 37% of 30-39 year olds experienced a complication.
- Acute complications were associated with reduced ability to self-care at discharge – with 13% of 19-29 year olds and 17% of 30-39 year olds unable to look after themselves once discharged from hospital.
- The complications were different to long-haul COVID symptoms in COVID-19 patients who were not hospitalized.
The patient’s inability to look after themselves, places substantial strain and the individual’s quality of life and ability to support themselves, as well a health care services thereafter.
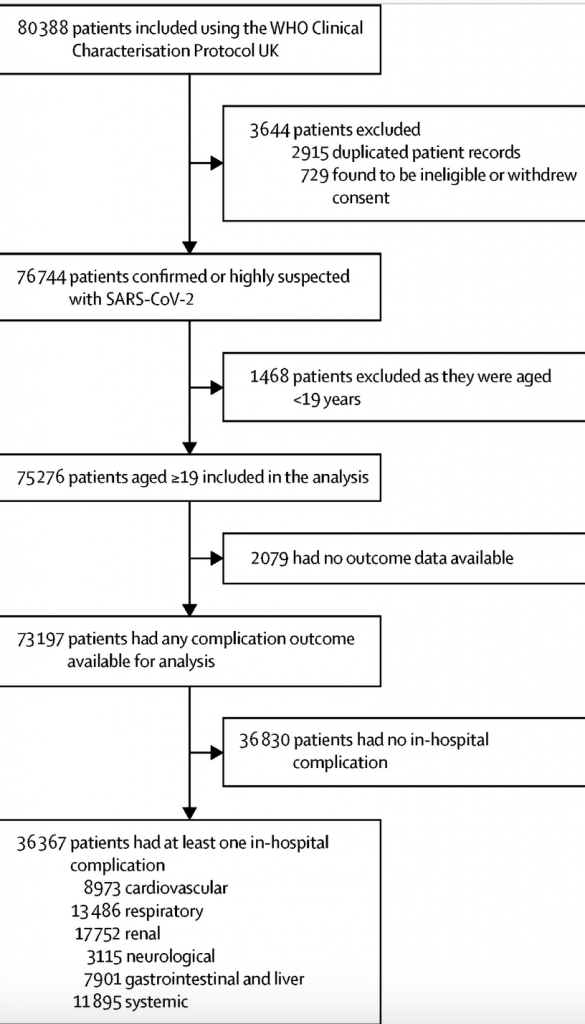
Lancet Study Data on hospitalized COVID-19 patients developing complications
The study looked at cases between 17 January and 4 August 2020 before vaccines were widely available, and new variants of the virus had not arisen. However, the authors note that their findings remain relevant in dispelling suggestions that COVID-19 presents no risk to younger healthy adults, many of whom remain unvaccinated.
“This work contradicts current narratives that COVID-19 is only dangerous in people with existing comorbidities and the elderly. Dispelling and contributing to the scientific debate around such narratives has become increasingly important, said Chief Investigator and joint senior author of the study, Professor Calum Semple, University of Liverpool, UK.
Data were collected by nurses and medical students, and included the participants’ age, sex at birth, health measures when hospitalized, and comorbidities (such as asthma, chronic cardiac disease, chronic hematological disease, chronic kidney disease, chronic neurological disease, chronic pulmonary disease, HIV/AIDS, cancer, liver disease, obesity, rheumatological disorders, and smoking).
In addition, they collected data on the respiratory, neurological, cardiovascular, renal, gastrointestinal and systemic complications participants experienced while in hospital [2]. Complications were assessed at multiple time points until discharge or, if the patient was not discharged, 28 days after hospitalization [3]. The study also investigated the ability of patients to look after themselves when discharged from hospital.
“Patients in hospital with COVID-19 frequently had complications of the disease, even those in younger age groups and without pre-existing health conditions. These complications could affect any organ, but particularly the kidney, heart and lungs. Those with complications had poorer health on discharge from hospital, and some will have long-term consequences. We now have a more detailed understanding of COVID-19 and the risks posed, even to younger otherwise healthy people,” said Joint senior author Professor Ewen Harrison from the University of Edinburgh, UK.
The most common complications were renal (affecting almost one in four people, 24%, 17,752), respiratory (affecting around one in five people, 18%, 13,486), and systemic (affecting one in six, 16%, 11,895). However, cardiovascular complications were reported in around one in eight participants (12%, 8,973), and neurological (less than one in 20, 4%, 3,115), and gastrointestinal or liver (less than 1%, 7,901) complications were also reported. Specifically, acute kidney injury, probable acute respiratory distress syndrome, liver injury, anaemia, and cardiac arrhythmia were the most common complications.
The incidence of complications rose with increasing age, occurring in 39% (3,596 of 9,249) of 19-49 year olds, compared to 51% (32,771 of 63,948) of people aged 50 and older. Going up the age ranges, 27% of 19-29 year olds hospitalised with COVID-19 developed a complication, 37% of 30-39 year olds, 43% of 40-49 year olds, 49% of 50-59 year olds, 54% of 60-69 year olds, 52% of 70-79 year olds, 51% of 80-89 year olds, and 50% of people aged 90 or over (see Table 1 in full report).
- Complications were more common in men compared with females, with males aged older than 60 years the most likely group to have at least one complication (women aged under 60 years: 37% [2,814 of 7,689] and men 49% [5,179 of 10,609]; women aged 60 years and over: 48% [11,707 of 24,288] and men 55% [16,579 of 30,416]).
- People of white, South Asian, and East Asian ethnicities had similar rates of complications, but rates were highest in Black people (58% [1,433 of 2,480] in Black patients vs 49% [26,431 of 53,780] in white patients – see Table 1).
- Following hospitalization, 27% (13,309 of 50,105) of patients were less able to look after themselves than before COVID-19, and this was more common with older age, being male, and in people who received critical care.
“It is important that with the high risk of complications and the impact these have on people, that complications of COVID-19, not just death, are considered when making decisions on how best to tackle the pandemic. Just focusing on death from COVID-19 is likely to underestimate the true impact, particularly in younger people who are more likely to survive severe COVID-19,” says Aya Riad, joint co-author from the University of Edinburgh, UK.
Based on these rates, the authors say that policymakers and health-care planners should anticipate that large amounts of health and social care resources will be required to support those who survive COVID-19. This includes adequate provision of staffing and equipment – for example, provision of follow-up clinics for those who have sustained in-hospital complications such as acute kidney injury or respiratory tract infection.
Click Here for Full Text Study





