In the first retrospective cohort study of the functional medicine model, Cleveland Clinic researchers found that functional medicine was associated with improvements in health-related quality of life. The study was published in the Journal of the American Medical Association Network Open.
The two-year study examined 1,595 patients treated in Cleveland Clinic’s Center for Functional Medicine and 5,657 patients seen in primary care at a family health center, assessing health-related quality of life using PROMIS®, an NIH-validated questionnaire. PROMIS provides a measure of patients’ global physical and mental health that can be monitored over time, measuring factors like fatigue, physical function, pain, gastrointestinal issues, and emotional well-being.
The study investigated the association between the functional medicine model of care and health-related quality of life by comparing functional medicine patients with patients seen in a primary care setting.
Functional Medicine Model of Care
Researchers found that patients seen by the Center for Functional Medicine showed beneficial and sustainable improvements in their PROMIS global physical health. At 6 months, patients seen by the Center for Functional Medicine exhibited significantly larger improvements in PROMIS global physical health compared to those seen in a primary care setting.
Approximately 31% of patients seen by the Center for Functional Medicine improved their PROMIS global physical health scores by 5 points or more, which is a clinically meaningful change and a noticeable effect on daily life.
Twenty-two percent of primary care patients improved their scores by 5 points or more. At 12 months, patients seen by the Center for Functional Medicine showed improvement similar to that observed at 6 months, but these were not significant when compared with the improvements seen in primary care patients.
To examine this further, researchers evaluated continuous changes over time in PROMIS global physical health in a smaller group of patients seen by the Center for Functional Medicine at both 6 and 12 months and demonstrated improvements in PROMIS global physical health that were significantly larger compared to patients seen in a primary care setting.
Researchers believe that reasons for the improvements in health-related quality of life shown in the functional medicine patients include differences in the functional medicine model itself, the types of patients seeking functional medicine, and treatment adherence or belief in the model of care. Future prospective studies are needed to examine the functional medicine model of care and long-term outcomes.
“This is a first-of-its-kind study to evaluate the impact of the functional medicine model of care on patients’ health-related quality of life. In the past, evidence to support the model has been primarily anecdotal, published as case reports or based on specific, targeted interventions used as part of the functional medicine approach, such as nutritional changes,” said Michelle Beidelschies, Ph.D., director of Research and Education for the Cleveland Clinic Center for Functional Medicine and the lead author of the study.
“Functional medicine practitioners have suggested that their patients are improving with a systems-based approach to chronic disease. Now, they have evidence that their approach is associated with improved quality of life.” ~ Michelle Beidelschies, PhD
Patients seen in the primary care setting center had a higher median income, higher mean baseline PROMIS scores and a higher prevalence of diabetes and hypertension.
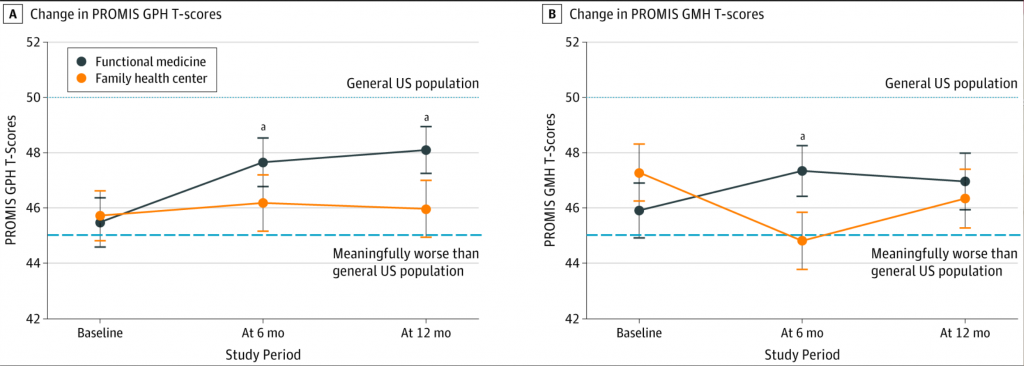
A, Continuous change in PROMIS GPH T-scores at baseline, 6 months, and 12 months in propensity score–matched patients (n = 91) in the functional medicine and family health care centers with scores at each time point. B, Continuous change in PROMIS GMH T-scores at baseline, 6 months, and 12 months in propensity score–matched patients (n = 97) in the functional medicine and family health care centers with scores at each time point. Change of 5 or more points was considered clinically meaningful on PROMIS Global Health T-score scales. Vertical lines represent SEs.
aSignificant between-group differences, P < .05.
As is well known by the integrative medical community, functional medicine looks at the body as a whole and focuses on the root causes of disease rather than an isolated set of symptoms. It’s based on the evidence that lifestyle factors – such as nutrition, sleep, exercise, stress levels, relationships, and genetics – are major contributors to chronic disease.
In 2014, Cleveland Clinic became the first academic medical center to open a Center for Functional Medicine. Cleveland Clinic’s Center for Functional Medicine requires that all new patients see a registered dietitian and health coach, in addition to a provider as part of their initial visit, which typically lasts about 60 to 75 minutes. Patients also have the option to meet with a behavioral health therapist as part of any visit.





