QUESTION: At what age and what circumstances or presenting pathologies or family history with certain pathologies should one undergo genetic testing? For instance, let’s say a patient had a grandparent who had colitis and died in his 70s from an adenocarcinoma, but his parents did not have any colitis or intestinal disorders. And, a colonoscopy at age 55 was negative for polyps. What do you suggest in regard to genomics testing and evaluation a patient in this situation.
~Ralph Nigro, ND, Natural Health Solutions
 ANSWER: Roberta Kline MD FACOG, and, Joe Veltman, PhD FAAIM DCCN, founders Genoma International: Dr. Nigro ‘s question, as we interpret it, happens to be two different questions; we cover each separately below, but this highlights the confusion that exists between the terms, genetic and genomic testing.
ANSWER: Roberta Kline MD FACOG, and, Joe Veltman, PhD FAAIM DCCN, founders Genoma International: Dr. Nigro ‘s question, as we interpret it, happens to be two different questions; we cover each separately below, but this highlights the confusion that exists between the terms, genetic and genomic testing.
The first question concerns what age, circumstances, presenting pathologies or family history of certain pathologies would a clinician recommend genetic testing for an inherited mutation passed from one generation to another. The example he references involves a patient whose grandparent who had colitis– I am assuming he is referring to ulcerative colitis (UC)–and died from adenocarcinoma in his 70s. Yet, the patient’s parents did not have UC or intestinal disorders. The patient, himself, had a colonoscopy at age 55 and was negative for polyps and is wondering if genetic testing would identify whether he is at risk for the inherited form of UC.
Here is what we know about UC today:
Familial Connection / UC is a chronic, pro- inflammatory disorder affecting primarily the colon. This disease runs in families especially among close relatives. A family history of the UC is the bigger risk factor the condition. According to the latest research, between 10 to 25 % of people with UC have a parent or sibling with IBD (UC or Crohn’s disease). Interestingly, UC that affects multiple family members often starts at an earlier age than it does with people with no family history of the condition.
Identical Twin Studies / To determine to what degree inherited genes play a role, identical twin studies showed that if one twin has UC, the other twin has 16 % higher risk for the disease. In contrast, fraternal twin studies found the risk to be about 4 %.
Ethnicity / UC has a higher prevalence in Caucasians and Ashkenazi Jews compared to other ethnic groups, suggesting that the genes responsible for UC are more prevalent among individuals of European descent.
GWAS / The most recent and largest genome wide association study (GWAS) for IBD, involving 75,000 patients and controls, established an association with 163 gene loci. The disease variance explained by the 163 gene loci only amounted to 13.6 % for Crohn’s disease and 7.5 % for UC.
As with most chronic, multi-factorial diseases like UC, finding a single inherited, loss of function gene that consistently confers the disease across generations and multiple ethnic populations is highly unlikely.
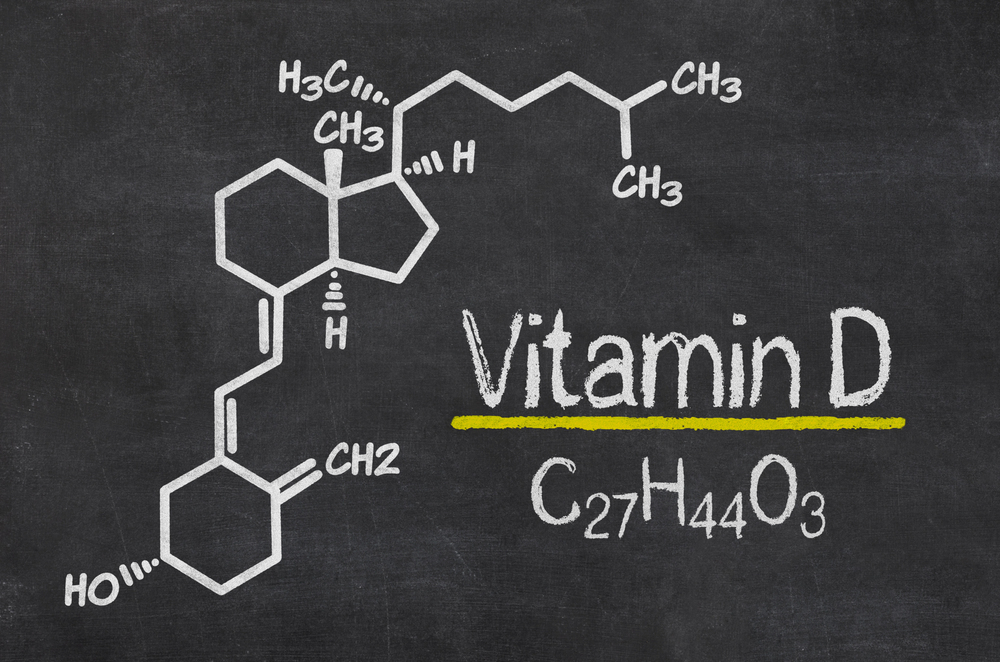
UC is best characterized as a polygenic disorder, in which multiple gene SNPs (single nucleotide polymorphisms) predispose an individual to a pro-inflammatory condition in the colon. Development of disease, including UC, is depending on interaction of these gene SNPs with important environmental factors. These factors include smoking; the health of the microbiome; food intolerances/sensitivities/allergies; OTC medications, dietary insufficiencies, deficiencies or excesses; emotional stressors.
This leads into the second question: do we have suggestions regarding genomic testing and how best to evaluate this patient with this history for UC?
ANSWER, BK, JV: We would suggest comprehensive genomic testing that evaluates as many genes as possible within the following biological systems of the patient, which can be found in both our Immuno-Health and Ultimate Wellness genomic test panels:
- Inflammation
- Detoxification
- Oxidative Stress
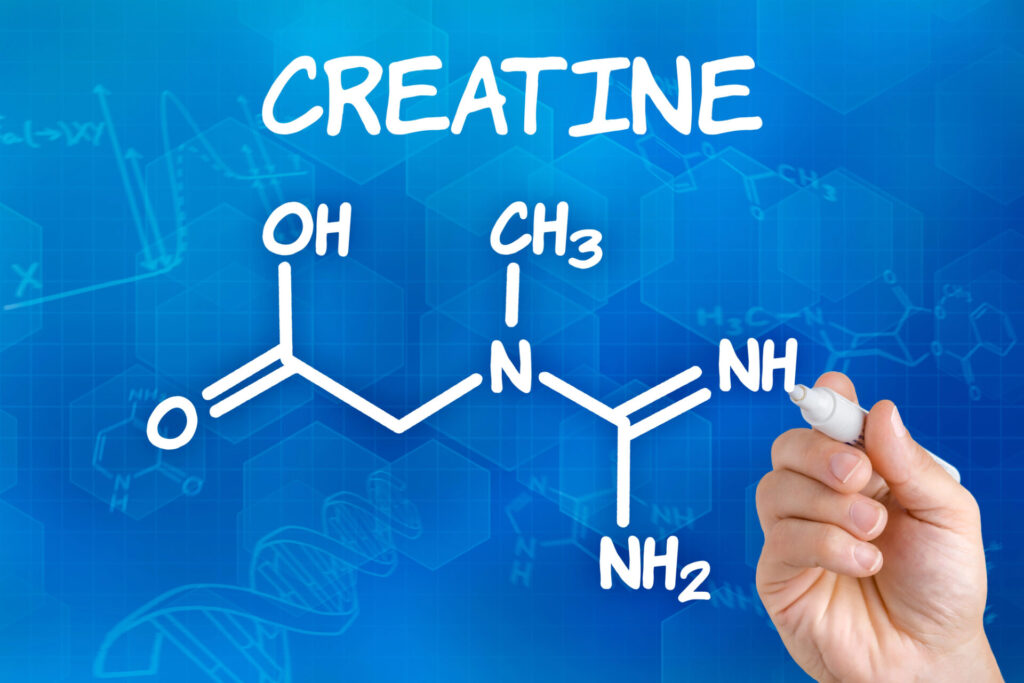
- Nutrient Digestion, Absorption, Transport and Utilization
- Stress Response
It’s important to integrate the patient’s clinical history with the genomic testing to direct with more precision the effective interventions as well as additional lab testing needed. This could include stool testing for microbiome diversity, pathogens, markers of inflammation and malabsorption; it may also indicate the need for systemic lab testing to assess inflammation, oxidative stress, detoxification and/or micronutrient status.
Selected References: