It is commonly known that colorectal cancer risk is greater for first-degree relatives (FDR) of patients with colorectal cancer than the general population. Screening guidelines recommend a colonoscopy every 5 or 10 years beginning at the age of 40, which is dependent on whether colorectal cancer index-case is diagnosed at <60 or ≥60 y, respectively. Previous studies on whether the risk of neoplastic lesions have been inconclusive. This new study was designed to establish a better indication of risk of advanced neoplasia (three or more non-advanced adenomas, advanced adenoma, or invasive cancer) in FDR of patients with colorectal cancer compared to average-risk individuals (i.e., asymptomatic adults 50 to 69 y of age with no family history of colorectal cancer). Published May 3, 2016, PLOS medicine.
 This study analyzed data from 8,498 individuals who underwent their first colonoscopy screening between 2006 and 2012 at six Spanish tertiary hospitals. Within this cross sectional data set, 3,015 were defined as asymptomatic FDR of patients with colorectal cancer (“familial-risk group”) and 3,038 as asymptomatic with average-risk for colorectal cancer (“average-risk group”).
This study analyzed data from 8,498 individuals who underwent their first colonoscopy screening between 2006 and 2012 at six Spanish tertiary hospitals. Within this cross sectional data set, 3,015 were defined as asymptomatic FDR of patients with colorectal cancer (“familial-risk group”) and 3,038 as asymptomatic with average-risk for colorectal cancer (“average-risk group”).
The familial stratified group was defined as follows:
- Familial-risk group was stratified as one FDR, with one family member diagnosed with colorectal cancer at ≥60 y (n = 1,884) or at <60 y (n = 831), and
- As two FDR, with two family members diagnosed with colorectal cancer at any age (n = 300).
Multiple logistic regression analysis was used for between-group comparisons after adjusting for potential confounders (age, gender, and center). Compared with the average-risk group, advanced neoplasia was significantly more prevalent:
- In individuals having two FDR with colorectal cancer (odds ratio [OR] 1.90; 95% confidence interval [CI] 1.36–2.66, p < 0.001),
- But not in those having one FDR with colorectal cancer diagnosed at ≥60 y (OR 1.03; 95% CI 0.83–1.27, p = 0.77) and <60 y (OR 1.19; 95% CI 0.90–1.58, p = 0.20).
- After the age of 50 y, men developed advanced neoplasia over two times more frequently than women and advanced neoplasia appeared at least ten y earlier.
- Fewer colonoscopies by 2-fold were required to detect one advanced neoplasia in men than in women.
According the researchers, the key findings included the following:
- The number of index-cases was 2,474 (median age 66.2 y). Of these, 1,399 (56.5%) were male and 786 (31.7%) were aged <60 y at diagnosis of colorectal cancer. Siblings with colorectal cancer predominated among individuals having two FDR affected compared to individuals having only one FDR with colorectal cancer (77.7% versus 25.5%, p < 0.001) Compared to average risk individuals, mean age of the familial-risk individuals was lower (51.8 ± 9.0 versus 59.3 ± 5.5 y, p < 0.001), as was the proportion of men (41.3% versus 47.6%, p < 0.001), as shown in Excerpt from the study.
- Men and women having two FDR with colorectal cancer showed a significantly greater risk of advanced adenomas and advanced neoplasia than those with average-risk.
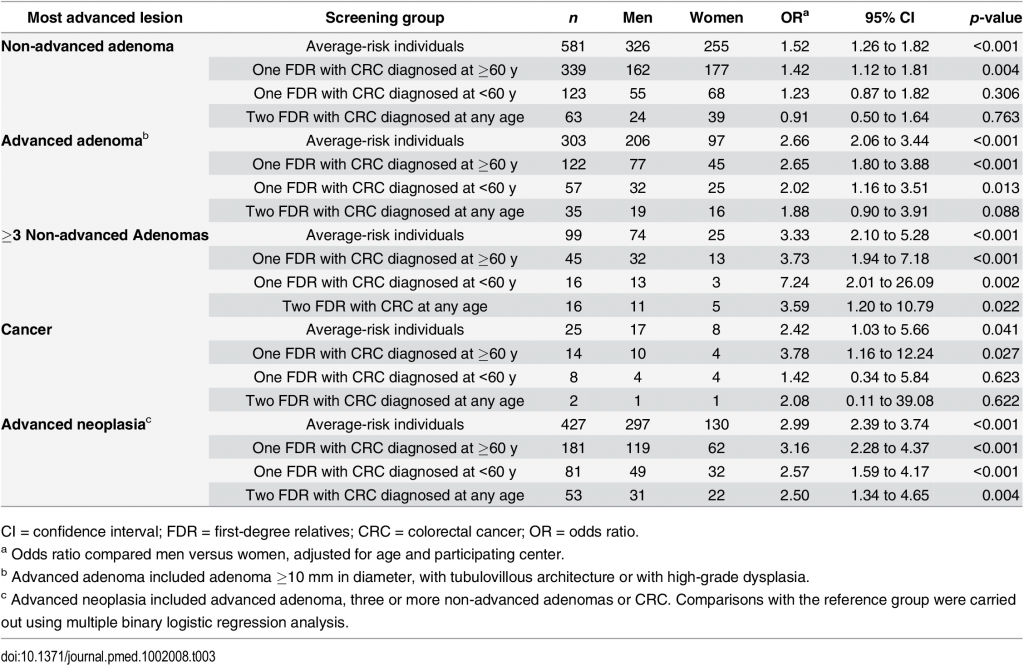
- In contrast, men and women having one FDR with colorectal cancer showed a similar risk of these lesions to average-risk individuals, regardless of index-case age at diagnosis of colorectal cancer. The risk of advanced neoplasia was almost 3-fold higher and appeared at least 10 y earlier in men than in women in both the familial- and average-risk groups. See Table 3 below.
- The number of colonoscopies needed to detect one advanced neoplasia was 2-fold higher in women than in men at all ages in both cohorts. Taken together, our results support the notion that screening colonoscopy may be delayed at least 10 y in women having one or even two FDR with colorectal cancer, as has been shown for women in the average-risk population.
CONCLUSION
“Men and women having two FDR with colorectal cancer showed a significantly greater risk of advanced adenomas and advanced neoplasia than those with average-risk. In contrast, men and women having one FDR with colorectal cancer showed a similar risk of these lesions to average-risk individuals, regardless of index-case age at diagnosis of colorectal cancer. The risk of advanced neoplasia was almost 3-fold higher and appeared at least 10 y earlier in men than in women in both the familial- and average-risk groups.”
TABLE 3