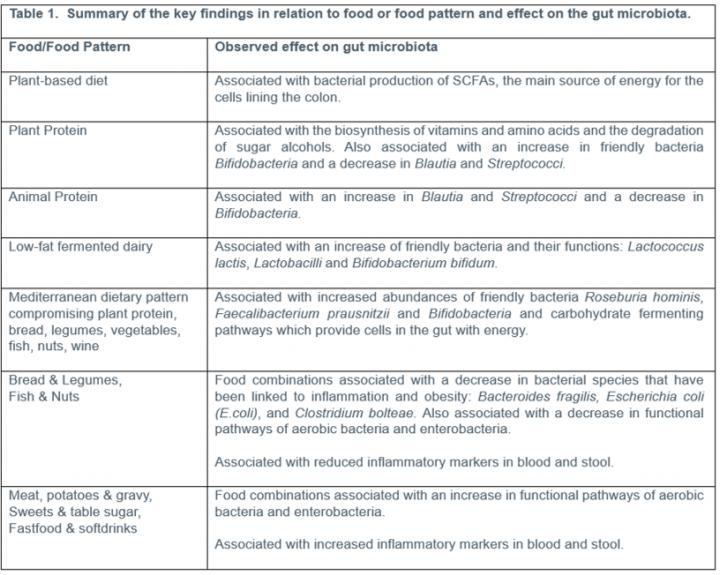
Researchers from the University Medical Center Groningen, The Netherlands have found that certain foods including legumes, bread, fish, nuts, and wine are associated with a better gut microbiome that aids the biosynthesis of essential nutrients and the production of short-chain fatty acids (SCFAs), the main source of energy for cells lining the colon. The findings support the idea that the diet could be an effective management strategy for intestinal diseases, through the modulation of gut bacteria.
The experts observed four study groups, the general population, patients with Crohn’s disease, ulcerative colitis and those with irritable bowel syndrome (IBS). The researchers analyzed a stool sample provided by each participant to reconstruct the host’s microbiota and compared this with the results of a food frequency survey. The results identified 61 individual food items associated with microbial populations and 49 correlations between food patterns and microbial groups.
The experts found that:
- Dietary patterns rich in bread, legumes, fish, and nuts, were associated with a decrease in potentially harmful, aerobic bacteria. Higher consumption of these foods was also associated with lower levels of inflammatory markers in the stool that are known to rise during intestinal inflammation.
- A higher intake of meat, fast foods or refined sugar was associated with a decrease in beneficial bacterial functions and an increase in inflammatory markers.
- Red wine, legumes, vegetables, fruit, cereals, fish and nuts were associated with a higher abundance of bacteria with anti-inflammatory functions.
- Plant-based diets were found to be associated with high levels of bacterial SCFA production, the main source of energy for cells lining the colon.
- Plant protein was found to help the biosynthesis of vitamins and amino acids, as well as the breaking down of sugar alcohols and ammonium excretion.
- Animal-derived and plant-derived protein showed opposite associations on the gut microbiota.
Gut health and microbiota
Links have also been made to obesity and a lack of diversity of the microbiota has been shown in people with inflammatory diseases such as IBD, psoriatic arthritis, diabetes, atopic eczema, celiac disease, and arterial stiffness. In these diseases, certain diets have been implicated as risk factors and this new research indicates that gut microbiota may help explain the link between diet and disease.
Commenting, lead researcher Laura Bolte said, “We looked in depth at the association between dietary patterns or individual foods and gut microbiota. Connecting the diet to the gut microbiome gives us more insight into the relation between diet and intestinal disease. The results indicate that diet is likely to become a significant and serious line of treatment or disease management for diseases of the gut, by modulating the gut microbiome.”
To conclude the dietary recommendations that could be derived from the study, Bolte added, “A diet characterized by nuts, fruits, greater vegetable and legume intake than animal protein, combined with moderate consumption of animal-derived foods like fish, lean meat, poultry, fermented low-fat dairy, and red wine, and a lower intake of red meat, processed meat, and sweets, is beneficially associated with the gut ecosystem in our study.”