Aging adults are the fastest growing age group in Western societies. As such, the risk of disability that prevents older  individuals from taking care of daily basic functions is high. In this study, published in Journal of the American Geriatrics Society, researchers explored how protein intake helps people maintain independence. The results show that physicians may want to suggest higher protein intake for aging patients.
individuals from taking care of daily basic functions is high. In this study, published in Journal of the American Geriatrics Society, researchers explored how protein intake helps people maintain independence. The results show that physicians may want to suggest higher protein intake for aging patients.
To learn more about protein intake and disability in older adults, the research team used data from the Newcastle 85+ Study conducted in the United Kingdom (UK). Researchers approached all people turning 85 in 2006 in two cities in the UK for participation. At the beginning of the study in 2006-2007, there were 722 participants, 60 percent of whom were women. The participants provided researchers with information about what they ate every day, their body weight and height measurements, their overall health assessment (including any level of disability), and their medical records.
The researchers learned that more than one-quarter (28 percent) of very old adults in North-East England had protein intakes below the recommended dietary allowance. The researchers noted that older adults who have more chronic health conditions may also have different protein requirements. The researchers examined the impact of protein intake on the increase of disability over five years.
The protein RDA for all adults is 0.8 g/kg BW/d, but there are proposals to increase it to at least 1.0 g/kg BW/d for older adults. Accordingly, protein intake was expressed as g/kg aBW/d, below or above 0.8 g/kg aBW/d and below or above 1.0 g/kg aBW/d. The disability score was calculated at baseline and after 18, 36, and at 60 months of follow‐up (See Figure 1). Ability to perform activities involved predominantly lower limb mobility (getting around the house, getting in and out of a chair, shopping for groceries, going up and down stairs and walking at least 400 yards (370 m).
FIGURE 1
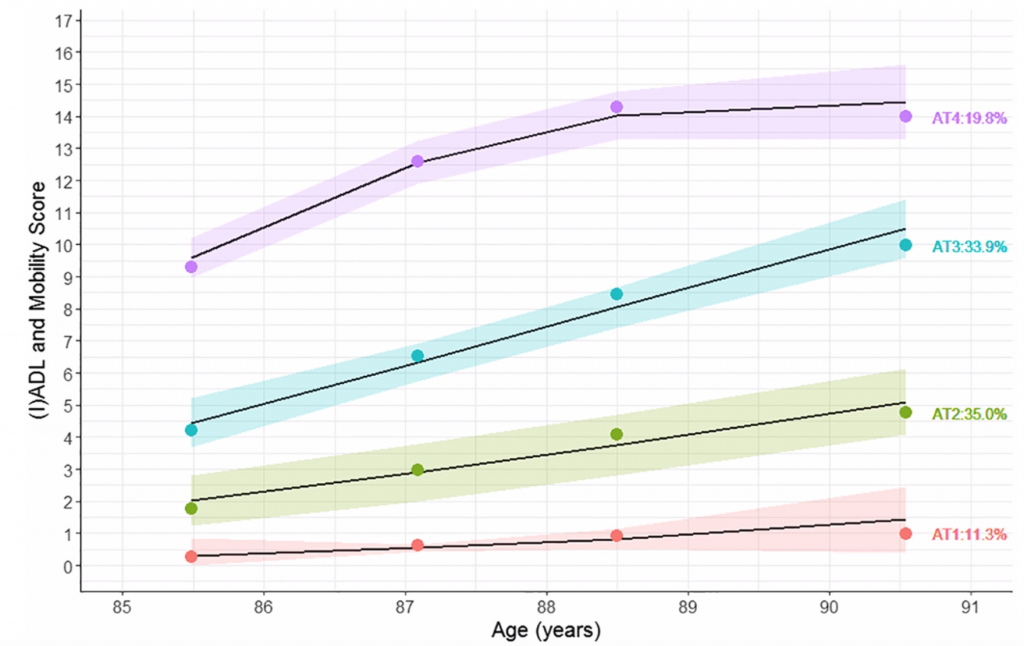
Consistent with the hypothesis, researchers showed that people aged 85.0 years old (± 0.5) with greater protein intake (g/kg aBW/d) were more likely to have fewer disabilities at baseline and shallower disability trajectories over the subsequent 5 years, after adjusting for covariates.
Participants who ate more protein at the beginning of the study were less likely to become disabled when compared to people who ate less protein.
Dr. Nuno Mendonca, the principal author of the study, said: “Our findings support current thinking about increasing the recommended daily intake of protein to maintain active and healthy aging.”
The researchers note that a sustained increase in intake of 0.1 g of protein/kg aBW/d (7 g/d of protein for a 70‐kg individual, e.g., equivalent to 1 glass [200 mL] of semi-skim milk) increased the chance of having a shallow disability trajectory (AT1) by 20% and a mild disability trajectory (AT2) by 13%. The protective effect was more pronounced in participants with protein intake of 1.0 g/kg aBW/d or more.
The researchers say that this observation provides objective evidence in support of recommendations from groups such as, PROT‐AGE and the European Society for Clinical Nutrition and Metabolism study group, who have proposed an increase in the protein RDA for older adults from 0.8 to 1.0 to 1.2 g/kg per day.
Conclusion/ In models adjusted for socioeconomic, health, and lifestyle factors, in the oldest adults, higher protein intake, especially 1.0 g/kg aBW/d or greater, was associated with a shallower disability trajectory over the following 5 years. The results support the consensus statements that protein intake in older adults should approximate 1.0 to 1.2 g/kg BW/d, which is within the acceptable macronutrient distribution range.
Source: Nuno Mendonça, Antoneta Granic, Tom R. Hill, Mario Siervo, John C. Mathers, Andrew Kingston, Carol Jagger. Protein Intake and Disability Trajectories in Very Old Adults: The Newcastle 85 Study. Journal of the American Geriatrics Society, 2018; DOI: 10.1111/jgs.15592