We recently reported an animal study showing that high-fructose corn syrup may be a contributing factor to the rising rates of colon and rectal cancer among young adults. A new observational study from The Lancet Gastroenterology & Hepatology journal looked at long-term data for colon and rectal cancer incidence in 21 population-based registries across Australia (1983-2012), Canada (1995-2014), Denmark (1978-2012), Ireland (1995-2013), New Zealand (1995-2014), Norway (1953-2014), and the UK (1995-2014). It shows that the incidence of colon and rectal cancer in adults younger than 50 years has increased substantially over the latest available 10-year period in certain high-income countries.
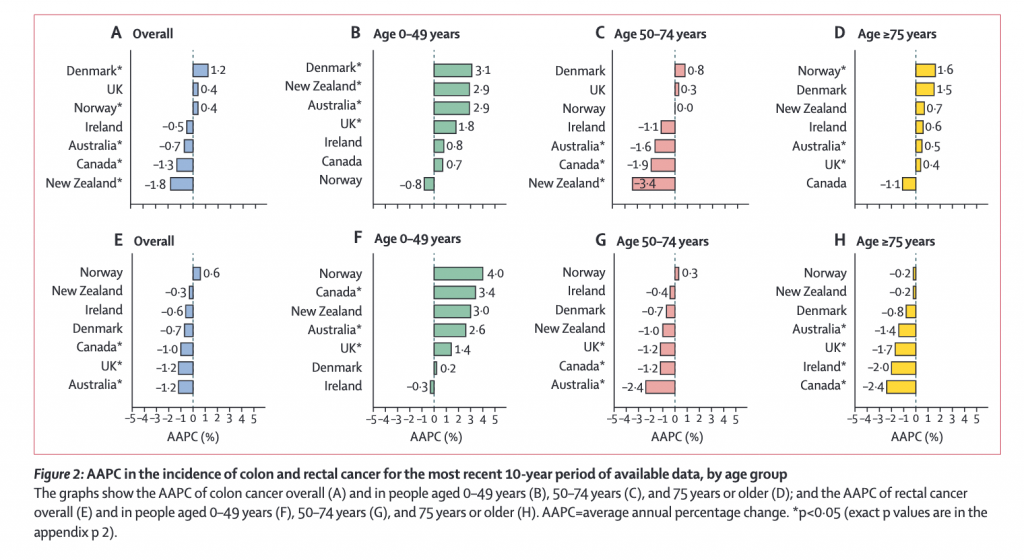
In The Lancet data, during the most recent 10-year period up until 2014, the incidence of colon cancer in people aged  0–49 years increased significantly each year in Denmark (by 3.1%), New Zealand (2.9%), Australia (2.9%), and the UK (1.8%). Significant increases in the incidence of rectal cancer each year were also noted in this age group in Canada (by 3.4%), Australia (2.6%), and the UK (1.4%). Increases in the incidence among adults under 50 were most pronounced for rectal cancer, particularly in the 20-29 age group, where rectal cancer incidence increased annually by 18.1% in Denmark and 10.6% in Norway over the past decade.
0–49 years increased significantly each year in Denmark (by 3.1%), New Zealand (2.9%), Australia (2.9%), and the UK (1.8%). Significant increases in the incidence of rectal cancer each year were also noted in this age group in Canada (by 3.4%), Australia (2.6%), and the UK (1.4%). Increases in the incidence among adults under 50 were most pronounced for rectal cancer, particularly in the 20-29 age group, where rectal cancer incidence increased annually by 18.1% in Denmark and 10.6% in Norway over the past decade.
Across the same time period, significant decreases in incidence of colon cancer per annum were observed in those aged over 50 in Australia (by 1.6%), Canada (1.9%), and New Zealand (3.4%) and of rectal cancer in Australia (2.4%), Canada (1.2%), and the UK (1.2%).
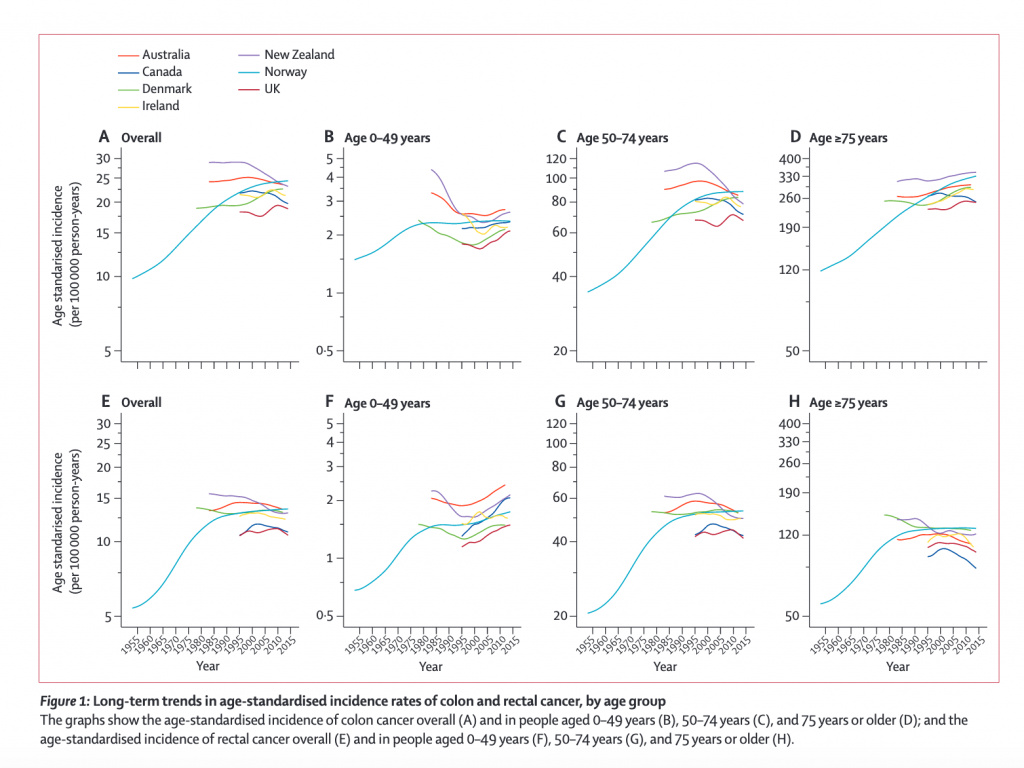
Trends in the incidence of colon and rectal cancer by age group showed diverging pattern (See Figure 1 and Figure 2 below):
- In people aged 0–49 years, the incidence of colon cancer increased significantly in Denmark (by 3·1%), New Zealand (2·9%), Australia (2·6%), and the UK (1·8%) over the most recent 10-year period (figure 2B), and these increases were more pronounced in women and girls than in men and boys
- In people aged 0–49 years, an increase in incidence was noted particularly for tumors occurring in the distal (left-side) colon (appendix pp 5, 11). In people aged 0–49 years, the incidence of rectal cancer increased significantly in Canada (by 3·4%), Australia (2·6%), and the UK (1·4%; figure 2F).
- Analyses by age subgroup showed that, among people aged 20–29 years, there were significant and large increases in the incidence of colon cancer in Denmark and Australia, and a significant decrease in incidence this age group in Canada (figure 3; appendix p 6).
- There was also a significant increase in the incidence of rectal cancer among people aged 20–29 years in Denmark. The increasing incidence of colon cancer was driven largely by increases in the incidence of distal colon cancer both overall (appendix pp 5–6, 11) and in people aged 20–29 years (appendix p 7).
Colorectal cancer is the third most common cancer worldwide, with an estimated 1·8 million new cases diagnosed and 881 000 deaths associated with the disease in 2018. This study is the first of its kind to comprehensively address and compare age-specific trends in the incidence of colorectal cancer, with its findings identifying divergent trends for different age groups.
“Although the incidence of colorectal cancer in adults younger than 50 years remains much lower compared with that in older age groups, our findings are of concern and highlight the need for action to counteract the rising burden of the disease in younger people. This rise in incidence among younger generations is likely to be driven in part by the changing prevalence of risk factors, such as obesity and poor diet. National programmes to promote healthy diets and physical activity might be the most efficient approach to ensure population-level changes.” ~ lead author of the study, Dr Marzieh Araghi from International Agency for Research on Cancer, Lyon
The authors of the study suggest that the decrease in incidence of colorectal cancer in people over 50 years old in most of the countries studied could be attributed to the introduction of routine screening programmes for premalignant polyps. In Australia, Canada, and the UK, where age-based screening began in 2006, overall decreases in incidence were more pronounced. In those countries where screening programmes began later, such as in Ireland (2012), Denmark (2014), Norway (2012, pilot programme only), and New Zealand (2017), overall rates have remained roughly stable.
“While population-based screening in people under 50 years old is not considered to be cost-effective due to relatively low incidence numbers, family history could help to identify younger people at high-risk of genetic susceptibility to colorectal cancer, for further assessment. However, future studies are needed to establish the root causes of this rising incidence to enable the development of effective preventive and early-detection strategies.” ~ Dr Araghi
Writing in a commentary, Professor Giulia Martina Cavestro from Vita-Salute San Raffaele University, Milan says, “Araghi and colleagues address the debate about lowering the age of screening. In 2018, the American Cancer Society recommended that screening for colorectal cancer should start at age 45 years for all adults. Such an approach is needed, but other initiatives should be endorsed alongside this decision. Furthermore, public awareness campaigns are essential to increase adherence to screening, and more gastroenterology units are likely to be needed. The lower age for screening should not be one-size-fits-all—personal and family history should be taken into account. Among the many risk factors, the importance of taking an accurate family history during a risk assessment cannot be overstated.”
Professor Cavestro is referring to an American Cancer Society study from 2013, showing that for adults ages 20 to 39, colon cancer incidence rates increased by 1% to 2% per year through 2013 in the United States. In adults 40 to 54, rates increased by 0.5% to 1% per year from the mid-1990s through 2013.
Rectal cancer incidence rates increased even longer and faster than colon cancer, rising about 3% per year from 1974 to 2013 in adults ages 20 to 29 and from 1980 to 2013 in adults ages 30 to 39. In adults ages 40 to 54, rectal cancer rates increased by 2% per year from the 1990s to 2013.
In terms of limitations, the researchers did not have access to individual-level data on risk factors and screening, so could not examine how changes to these factors interacted with trends in colorectal cancer over time. Furthermore, as noted in the linked commentary, there were only seven high-income countries included in this study; adding data from more countries could strengthen the conclusions on the changing epidemiology of colorectal cancer.
Conclusion/ The findings of rising incidence of colon and rectal cancer among young adults in high-income countries highlight the need for studies to establish the underlying causes and identify potential preventive and early-detection strategies.
Click Here for Full Text Study
Source: M Araghi et al. Colorectal cancer incidence on the rise among young adults in several high-income countries. Lancet Gastroenterol Hepatol 2019, Published online May 16, 2019 http://dx.doi.org/10.101/S2468-1253(19)30147-5