When running a routine glycosylated hemoglobin (A1C) test to track blood sugar levels, you may want to consider also using the test to identify individuals with advanced atherosclerosis. Though the test is used primarily for the diagnosis and management of prediabetes and diabetes, the glycosylated hemoglobin test can provide a useful estimate of atherosclerotic disease in individuals without diabetes or possible prediabetes. This is the main finding of a study carried out by scientists at the Centro Nacional de Investigaciones Cardiovasculares (CNIC), published in The Journal of American College of Cardiology (JACC).

The CNIC study used the blood-sugar measure in apparently healthy middle-aged individuals who did not have diabetes mellitus. They found when the test is used in combination with traditional risk factors (hypertension, dyslipidemia, and smoking), the glycosylated hemoglobin test more accurately distinguished between people at high and low risk of atherosclerotic disease.
Since the glycosylated hemoglobin diagnostic test is cheap, accessible, and widely used in daily clinical practice, it could therefore be used to calculate the degree of subclinical atherosclerosis in the general population, explained Dr. Xavier Rosselló, CNIC scientist and cardiologist at Hospital Universitario Son Espases in Palma de Mallorca.
The study included a cohort of 3,973 middle-aged individuals from the PESA (Progression of Early Subclinical Atherosclerosis) study, with no history of cardiovascular disease and with HbA1c in the non-diabetic range They were assessed for the presence and extent of subclinical atherosclerosis (SA) by 2-dimensional vascular ultrasound and noncontrast cardiac computed tomography.
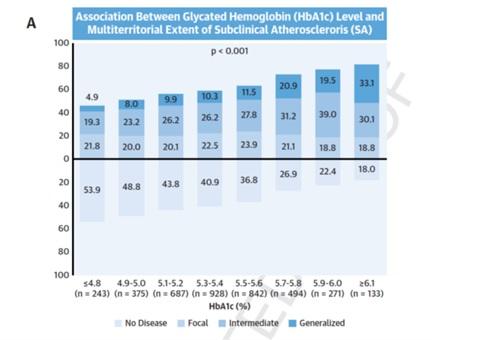
- After adjusting for established cardiovascular disease risk factors, HbA1c showed an association with the multi-territorial extent of SA.
- The association was significant in all pre-diabetes groups and even below the pre-diabetes cut-off (HbA1c 5.5% to 5.6% odds ratio: 1.36 [95% confidence interval: 1.03 to 1.80]; p = 0.033).
- High HbA1c was associated with an increased risk of SA in low-risk individuals (p < 0.001), but not in moderate-risk individuals (p = 0.335).
- Relative risk estimations using Systematic Coronary Risk Estimation or atherosclerotic cardiovascular disease predictors confirmed that inclusion of HbA1c modified the risk of multiterritorial SA in most risk categories.
“The glycosylated hemoglobin test was especially useful in identifying subclinical disease in participants classified at low risk according to traditional scores; it made less of a contribution to risk calculation for individuals who already had a moderate level risk according to other risk factors,” said Dr. Rosselló.
Since atherosclerosis is usually only detected at advanced stages, after it has already triggered a cardiovascular event such as a myocardial infarction or stroke, the new CNIC finding provides a simple way to increase the accuracy of cardiovascular risk ranking in individuals without diabetes with or without prediabetes.
According to CNIC General Director Dr. Valentín Fuster, this new information “will help to provide a more personalized assessment of cardiovascular risk at almost no additional cost, paving the way to personalized treatment plans principally focused on lifestyle changes, followed when necessary by treatment with antidiabetic drugs.”
The authors conclude that “this study establishes glycosylated hemoglobin as a mass-use biomarker because its greatest benefit is in individuals at low cardiovascular risk, who form the immense majority of the general population and account for most cardiovascular deaths in absolute terms.”
Click Here for Full Text Study
Source: Xavier Rossello, Sergio Raposeiras-Roubin, Valentin Fuster et al. Glycated Hemoglobin and Subclinical Atherosclerosis in People Without Diabetes,
Journal of the American College of Cardiology .Volume 77, Issue 22,
2021, Pages 2777-2791, doi.org/10.1016/j.jacc.2021.03.335.
The study was funded by the Instituto de Salud Carlos III (ISCIII, PI15/ 02019, PI17/00590, PI20/00819) and the European Regional Development Fund (ERDF) “A way to make Europe” and included scientists from the CIBER de Enfermedades CardioVasculares (CiberCV) research network. The study forms part of the collaborative PESA-CNIC-SANTANDER project, which is led by Dr. Fuster. Begun in 2010 and recently extended until 2030, the PESA-CNIC-SANTANDER study is one of the most important cardiovascular prevention studies in the world.




