An inadequate Omega-3 Index may be just as powerful in predicting early death as smoking. It’s a bold statement made in a research paper published in the American Journal of Clinical Nutrition. This study is based on data from the Framingham Heart Study.
The Framingham Heart Study provided unique insights into cardiovascular disease (CVD) risk factors and led to the development of the Framingham Risk Score based on eight baseline standard risk factors–age, sex, smoking, hypertension treatment, diabetes status, systolic blood pressure, total cholesterol (TC), and HDL cholesterol.
As is well known in the integrative health field, the risk of death from CVD can be reduced by changing behavioral factors such as unhealthy diet, physical inactivity, and use of tobacco and alcohol. The researchers in this study say biomarkers integrating lifestyle choices might help identify individuals at risk and be useful to assess treatment approaches, prevent morbidity, and delay death.
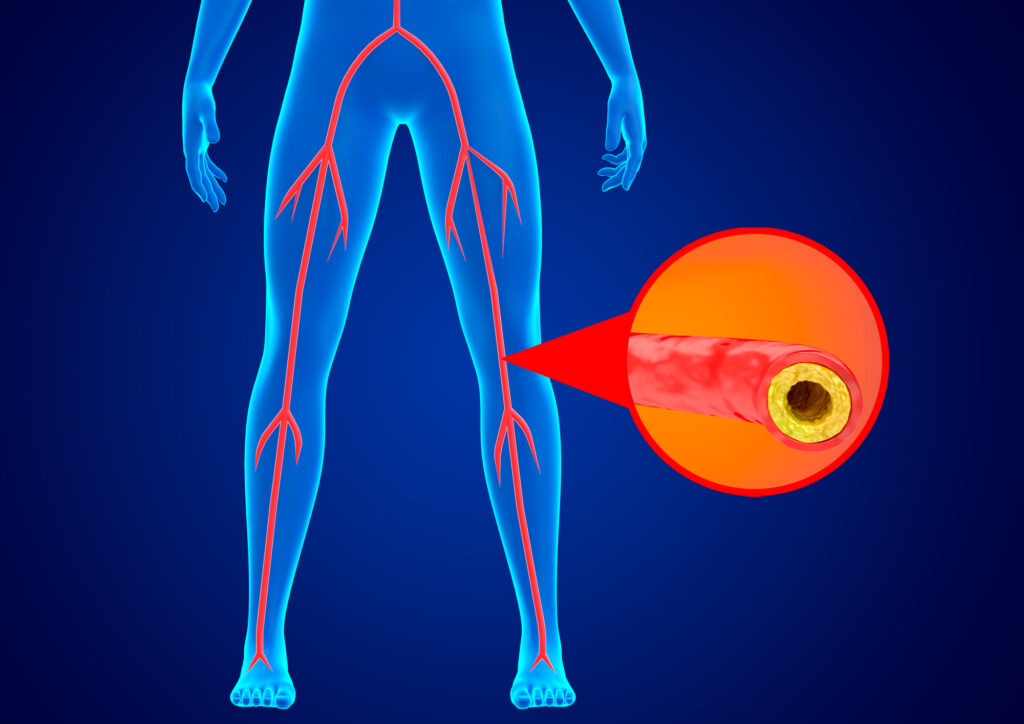
Among the diet-based biomarkers are fatty acids (FAs), whether measured in plasma or red blood cell (RBC) membranes. The FAs most clearly associated with reduced risk for CVD and for total mortality (i.e., death from any cause) are the omega-3 FAs, EPA and DHA, which are typically found in fish like salmon and herring, as well as omega-3 supplements like fish and algal oil.

In a 2018 report that included 2500 participants in the Framingham Offspring Cohort followed for a median of 7.3 years (i.e., between ages 66 and 73), the baseline red blood cell (RBC) EPA + DHA content [the omega-3 index (O3I)] was significantly and inversely associated with risk for death from all causes.
In fact, individuals with the highest Omega-3 Index were 33% less likely to succumb during the follow-up years compared with those with the lowest Omega-3 Index. Similar associations have been seen in the Women’s Health Initiative Memory Study, the Heart and Soul Study, and the Ludwigshafen Risk and Cardiovascular Health Study.
- An optimal Omega-3 Index is 8% or higher, an intermediate Omega-3 Index is between 4% and 8%.
- A low Omega-3 Index is 4% and below.
- Most Americans have an Omega-3 Index below 4%, which puts them a significantly higher risk of early death.
According to researchers in this study, the finding that any FA-based metric would have predictive power similar to that of the well-established standard risk factors was unexpected, and it suggests that RBC FAs–via imperfectly understood mechanisms–somehow reflects an in vivo milieu that consolidates into one measure the impact on the body of all these standard risk factors.
“It is interesting to note that in Japan, where the mean Omega-3 Index is greater than 8%, the expected life span is around five years longer than it is in the United States, where the mean Omega-3 Index is about 5%. Hence, in practice, dietary choices that change the Omega-3 Index may prolong life,” said Michael McBurney, PhD, FCNS-SCN, lead researcher in this study. “In the final combined model, smoking and the Omega-3 Index seem to be the most easily modified risk factors. Being a current smoker (at age 65) is predicted to subtract more than four years of life (compared with not smoking), a life shortening equivalent to having a low vs. a high Omega-3 Index.”
“The information carried in the concentrations of four red blood cell fatty acids was as useful as that carried in lipid levels, blood pressure, smoking, and diabetic status with regard to predicting total mortality,” said Dr. Bill Harris, who was also an author on this study. “This speaks to the power of the Omega-3 Index as a risk factor and should be considered just as important as the other established risk factors, and maybe even more so.”
Conclusion/ In this community-based population in their mid-60s, RBC FA patterns were as predictive of risk for death during the next 11 y as standard risk factors. Replication is needed in other cohorts to validate this FA fingerprint as a predictor of all-cause mortality.
Source: Michael I McBurney, Nathan L Tintle, Ramachandran S Vasan, Aleix Sala-Vila, William S Harris, Using an erythrocyte fatty acid fingerprint to predict risk of all-cause mortality: the Framingham Offspring Cohort, The American Journal of Clinical Nutrition, 2021;, nqab195, https://doi.org/10.1093/ajcn/nqab195
This work was supported in part by the Institute for the Advancement of Food and Nutrition Sciences (IAFNS) through an International Life Sciences Institute North America Lipid Committee grant. IAFNS is a nonprofit science organization that pools funding from industry collaborators and advances science through the in-kind and financial contributions from public and private sector participants.
The Fatty Acid Research Institute (FARI) is a non-profit research and education foundation. FARI was founded in order to accelerate discovery of the health effects of fatty acids, most notably, the long chain omega-3 fatty acids EPA and DHA. FARI researchers and scientists will focus single-mindedly on publishing high-quality research studies on the multiple relationships between fatty acid levels and human (and animal) health outcomes. These studies will improve the ability to predict risk for disease, and more importantly, suggest ways to reduce risk by changing our diets and/or supplementation regimens. http://www.faresinst.org