Researchers at the National Research University Higher School of Economics (HSE) discovered genetic predisposition to severe COVID-19. The results of the study were published in the journal Frontiers in Immunology.
Researchers from the HSE Faculty of Biology and Biotechnology – Maxim Shkurnikov, Stepan Nersisyan, Alexei Galatenko and Alexander Tonevitsky -together with colleagues from Pirogov Russian National Research Medical University and Filatov City Clinical Hospital (Tatjana Jankevic, Ivan Gordeev, Valery Vechorko) studied the interconnection between HLA-I genotype and the severity of COVID-19.
The studied T-cell immunity as the staging ground for cell immunity development and the presentation of virus peptides on the surface of infected cells. This is then followed by activation of T lymphocytes, which starts to kill the infected cells. The ability to successfully present virus peptides is largely determined by genetics.
In human cells, human leukocyte antigen class I (HLA-I) molecules are responsible for this presentation. The set of six such molecules is unique in every human and if the set of alleles detects the virus well, then the immune cells will detect and destroy the infected cells fast. However, if a person has a set that is bad at such detection, a more severe case of disease is more likely to be observed.
Using machine learning, they built a model that provides an integral assessment of the possible power of T-cell immune response to COVID-19:
- If the set of HLA-I alleles allows for effective presentation of the SARS-CoV-2 virus peptides, those individuals received low risk score,
- While people with lower presentation capability received higher risk scores (in the range from 0 to 100).
- To validate the model, genotypes of over 100 patients who had suffered from COVID-19 and over 400 healthy people (the control group) were analysed.
- The modeled risk score is highly effective in predicting severe COVID-19.
The clinical characteristics of the patients indicated that the HLA genotype, age, and underlying diseases were the most important risk factors for death. In the tested population, the median age of deceased patients was 73 years. Only 18 deceased elderly patients (21.2%) had no comorbidities.
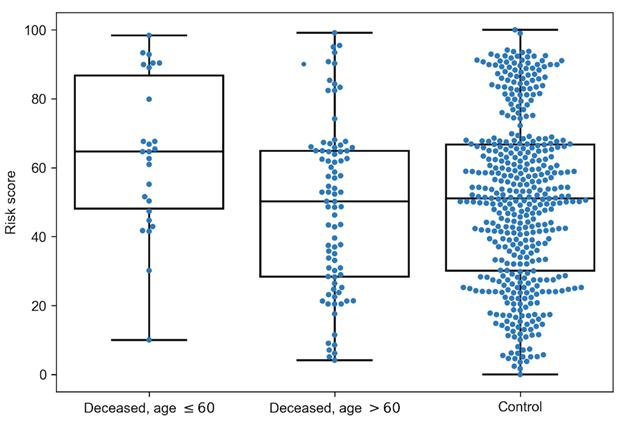
In addition to analyzing a Moscow population, the researchers used their model on a sample of patients from Madrid, Spain. The high precision of prediction was confirmed on this independent sample as well: the risk score of patients suffering severe COVID-19 was significantly higher than in patients with moderate and mild cases of the disease.
“In addition to the discovered correlations between the genotype and COVID-19 severity, the suggested approach also helps to evaluate how a certain COVID-19 mutation can affect the development of T-cell immunity to the virus. For example, we will be able to detect groups of patients for whom infection with new strains of SARS-CoV-2 can lead to more severe forms of the disease,” said Tonevitsky.
Click Here for Full Text Study