A new study by researchers at Icahn School of Medicine at Mount Sinai identifies different types of cardiac structural damage experienced by COVID-19 patients after myocardial injury that are associated with deadly conditions including heart attack, pulmonary embolism, heart failure, and myocarditis. These myocardial abnormalities are associated with higher risk of death among hospitalized patients.
The findings, published in the Journal of the American College of Cardiology, offer new insights that may help doctors better understand the mechanism of cardiac injury, leading to quicker identification of patients at risk and guidance on future therapies.
“Early detection of structural abnormalities may dictate more appropriate treatments, including anticoagulation and other approaches for hospitalized and post-hospitalized patients,” says author Valentin Fuster, MD, PhD, Director of Mount Sinai Heart and Physician-in-Chief of The Mount Sinai Hospital.
Myocardial Injury from COVID-19
The international, retrospective study expands on Mount Sinai’s previous research showing that myocardial injury (heart damage) is prevalent among patients hospitalized with COVID-19 and is associated with higher risk of mortality. That study focused on the patients’ levels of troponin–proteins that are released when the heart muscle becomes damaged–and their outcomes (higher troponin levels mean greater heart damage).
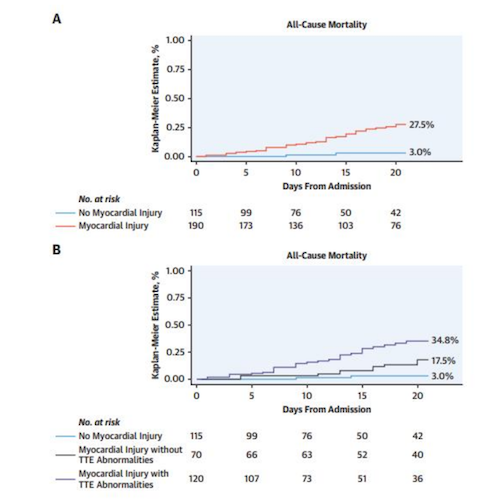
This new work looked at the presence of cardiac troponin elevations in combination with the presence of echocardiographic abnormalities, and found that the combination was associated with worse prognosis and mortality than troponin elevations alone.
ABSTRACT/ A total of 305 patients were included. Mean age was 63 years and 205 patients (67.2%) were male. Overall, myocardial injury was observed in 190 patients (62.3%). Compared with patients without myocardial injury, those with myocardial injury had more electrocardiographic abnormalities, higher inflammatory biomarkers and an increased prevalence of major echocardiographic abnormalities that included left ventricular wall motion abnormalities, global left ventricular dysfunction, left ventricular diastolic dysfunction grade II or III, right ventricular dysfunction and pericardial effusions.
- Rates of in-hospital mortality were 5.2%, 18.6%, and 31.7% in patients without myocardial injury, with myocardial injury without TTE abnormalities, and with myocardial injury and TTE abnormalities.
- Following multivariable adjustment, myocardial injury with TTE abnormalities was associated with higher risk of death but not myocardial injury without TTE abnormalities.
“This is one of the first studies to provide detailed echocardiographic and electrocardiographic data in hospitalized patients with COVID-19 and laboratory evidence of myocardial injury,” explains first and corresponding author Gennaro Giustino, MD, Cardiology Fellow at The Mount Sinai Hospital. “We found that among COVID-19 patients who underwent transthoracic echocardiography, these cardiac structural abnormalities were diverse and present in nearly two-thirds of patients.”
- Median age was 63 years and 67.2 percent were men. 190 patients (62.6 percent) had evidence of myocardial injury;
- 118 of them had heart damage at the time of hospitalization admission and 72 developed myocardial injury during hospitalization.
- Researchers found that patients with myocardial injury had more electrocardiographic abnormalities, higher inflammatory biomarkers, and an increased prevalence of TTE abnormalities when compared to patients without heart injury.
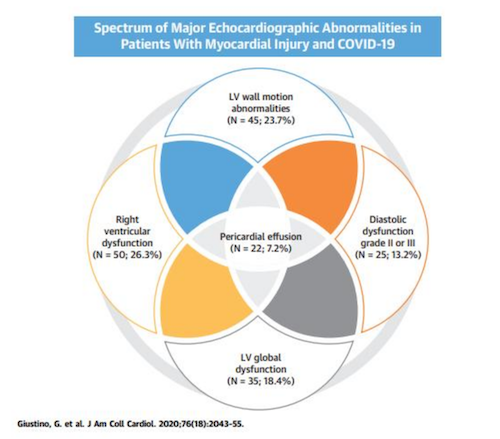
Scope and Diversity of Myocardial Injury
Abnormalities were diverse, with some patients exhibiting multiple abnormalities. 26.3 percent had right ventricular dysfunction (which can be associated with pulmonary embolism and severe respiratory failure), 23.7 percent had regional left ventricular wall motion abnormalities (which can be associated with heart attacks), 18.4 percent had diffuse left ventricular dysfunction (which can be associated with heart failure/myocarditis), 13.2 percent had grade II or III diastolic dysfunction (a condition leading to stiffer cardiac chambers), and 7.2 percent had pericardial effusions (extra fluid around the heart that causes abnormal pumping of the heart).
The study went on to look at in-hospital mortality and troponin elevation. It shows that troponin elevation was 5.2 percent among patients who did not have heart injury, compared to 18.6 percent for patients with myocardial injury but without echocardiographic abnormalities, and 31.7 percent for patients with myocardial injury who also had echocardiographic abnormalities. Researchers adjusted for other major complications from COVID-19 including shock, acute respiratory distress syndrome, and renal failure.
“Our study shows that an echocardiogram performed with appropriate personal protection considerations is a useful and important tool in early identification of patients at greater risk for COVID-19-related cardiac injury, who may benefit from a more aggressive therapeutic approach earlier in their hospitalization,” says corresponding author Martin Goldman, MD, Arthur M. and Hilda A. Master Professor of Medicine (Cardiology) at the Icahn School of Medicine at Mount Sinai.
“Additionally, because this is a new disease with lingering symptoms, we plan on following these patients closely using imaging to evaluate the evolution and hopefully resolution of these cardiac issues.”
“Echocardiograms have shown to be invaluable in providing critical information on patients who present with multiple cardiac complaints. Echocardiography is the only imaging modality that can be taken to the bedside and safely used for patients including those on ventilators,” says Lori Croft, MD, Associate Professor of Medicine (Cardiology) at the Icahn School of Medicine at Mount Sinai and Director of the Echocardiography Laboratory at The Mount Sinai Hospital. “Our findings will help guide care of Covid-19 patients during a critical time.”
Among patients with Covid-19 who underwent TTE, cardiac structural abnormalities were present in nearly two-thirds of patients with myocardial injury. Cardiac structural abnormalities included right ventricular dysfunction, left ventricular wall motion abnormalities, global left ventricular dysfunction, diastolic dysfunction and pericardial effusions. LV = Left Ventricular.
Conclusion/ Among patients with COVID-19 who underwent TTE, cardiac structural abnormalities were present in nearly two-thirds of patients with myocardial injury. Myocardial injury was associated with increased in-hospital mortality particularly if echocardiographic abnormalities were present.




