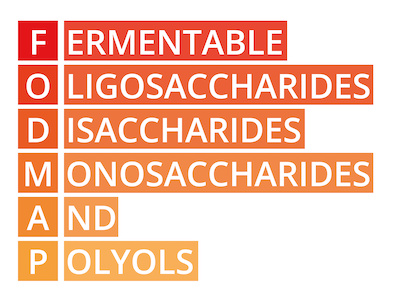
As the FODMAP diet grows in popularity, we need to be clear about what the research has revealed. There is a pervasive misunderstanding of what the FODMAP diet does and does not do, and how it should be used in a clinical setting.
The review study referenced in the article, Effects Of Regulating Intestinal Microbiota On Anxiety Symptoms: A Systematic Review, published in General Psychiatry, looked at twenty-one studies; fifteen of which were probiotic interventions and six were dietary interventions. Eleven studies in all showed a positive reduction of anxiety symptoms. Five of these studies were probiotic interventions and six were non-probiotic interventions. Of the five studies that were non-probiotic interventions, there were only two studies that look directly at a low FODMAP diet (LFD). [1]
Related Webinar with Angela Pifer:
Misconceptions of the Low FODMAP Diet: Facts, Myths & Patient Impact
One single-blind prospective study compared a 4-week LFD to the mNICE diet (a validated diet used in the treatment of IBS-D) in 84 subjects, and the results showed that the LFD intervention outperformed the mNICE diet, improving quality of life and anxiety scores. [2]
The second study compared a 4 week low FODMAP diet against yoga, and although both groups showed improved anxiety scores, the yoga intervention showed the most improvements.[3]
Two of the non-probiotic intervention studies looked at the effects of galactooligosaccharide (GOS) supplementation vs. resistant dextrin as the control. The fifth was labeled ‘nutrition intervention’ but neither the study, nor the specific interventions were made available for review.
When only two of the studies looked at a LFD and in one of the studies yoga was even more successful at reducing anxiety, should the FODMAP diet be singled out?
It is also clear that the author of the review study cited in the article in question is correlating a reduction in anxiety symptoms solely to the catch-all mechanism “regulation of intestinal microbiota.”
To say that probiotics merely regulate the intestinal microbiota is to grossly misconstrue the role that probiotics play in human health. They interact through a significant number of mechanisms: they produce short-chain fatty acids (SCFA) [4,5], enhance epithelia barrier integrity [6], modulate the immune system [7], influence hormone levels [8], produce enzymes [9], modulate gene expression [10] and studies have shown that probiotics can stimulate the enteric nervous system and affect gut transit time [11], and reduce visceral pain [12). Furthermore, L. reuteri has been shown to interact with the gut-brain axis in rats through the modulation of afferent sensory nerves that influence gut motility [13].
Although the mechanisms by which probiotics work are often underestimated, the mechanisms by which the FODMAP diet works are often overestimated. Studies have, with some consistently, shown that a FODMAP diet can alter digestive symptoms in IBS patients [14-17], yet it has not consistently been shown to do much else.
The exaggerated confidence given to the FODMAP diet, that it has the ability to favorably alter the intestinal microbiota, starve out organisms, or alter the immune system by reducing histamines, for example, are unfounded in the literature. The diet is being misrepresented across publications, by practitioners and over social media, and in chat rooms.
When a study says “FODMAP DIET” what are they actually testing?
If you search the term ‘low FODMAP’ in Pubmed.gov, the results returned will include a wide variety of dietary intervention methods, all under the umbrella term ‘low FODMAP.’ As with most investigative feeding studies, the methods are far from uniform across the studies.
Some studies use a true dietary intervention, comparing a low FODMAP diet (LFD) and a high FODMAP diet (HFD). Some provide the food, but most are instructing the subjects on the diet (ranging from 10 minutes of instruction to 3 sessions with a dietitian). The diet is then self-followed and adherence is self-reported. Generally, a HFD is equivalent to 50 grams of FODMAP a day, and a LFD is equivalent to 1.2-9 grams of FODMAP a day (the majority of studies use a 7-9 gram per day range).
Some studies place participants on 14-16 grams of fructooligosaccharides (FOS) or galactooligosaccharides (GOS) for the HFD arm. Others compare a LFD diet to FOS alone. In some FODMAP studies, dextrin is used as the control, where a LFD + 16 grams per day of dextrin is compared to a LFD + 16 grams per day FOS. [18]
When we look closely at the studies on FODMAP, and their proposed effects on the microbiota and the immune system, the findings are inconsistent at best. What is agreed upon is that LFD helps to alter symptoms of bloating, diarrhea and quality of life, but even these studies have issues with quality, “All trials had high risk of bias (only one double‐blinded), intervention periods ranged from 2 days to 6 weeks with one including a 6 month follow‐up. …control diets were heterogeneous with limited established efficacy.” [19]
Some studies are also mislabeling the benefits of a LFD. In the article, “Is A Low FODMAP Diet Dangerous?,” the author states, “Shepherd et al. [20] at 14-month follow-up, found 77% of patients adherent to the (LFD) with 76% reporting significant improvement in abdominal symptoms” and yet, the Shepard et al. study referenced only altered fructose, which should not be misconstrued as a low FODMAP dietary intervention. [21]
What are we as practitioners trying to acheive by using an LFD?
You Want to Starve Out the Organisms?
Methane levels do not increase, nor decrease in response to a LFD nor HFD intervention, respectively, in ALL studies where this is measured. [22, 23, 29-31] There are three studies that show a change in hydrogen. Before I discuss these studies, let’s look at the Lactulose Breath Test (LBT) and how this test was validated for use.
The LBT is a diagnostic tool to detect levels of excess hydrogen and methane that is produced when the consumed test substrate, lactulose, passes by higher than normal levels of organisms in the small intestine (bacteria and archaea are able to digest and ferment this sugar, but we cannot). The excess gas produced exchanges across the intestinal tract, into the blood and then circulates and moves out through our lungs – where it is measured in breath samples.
This test is a validated laboratory test when, and only when, the subject has properly prepped for this test. This includes a 12 hour food prep, that occurs 24 hours prior to the test, of only fish, eggs, chicken, white rice and white bread (the latter two are allowed because they digest rapidly in the upper section of the small intestine). Then the subject fasts for 12 hours, and then waits two hours after getting out of bed in the morning (because morning breathing is more shallow) to take a baseline measure. The baseline measure is a control marker for the lab, to show that the test prep was done properly.
Then a standard dose of lactulose is consumed and depending on the lab, the subject is instructed to collect breath samples in 15 to 30 minute increments, for 90-180 minutes.
The proper 12 hour food prep reduces fermentation potential of the organisms that reside in the large intestine, whereby, we are able to get a clearer measure of gases in the small intestine as the lactulose substrate moves past the organisms.
If prepping incorrectly, this is simply a measure of the fermentation of food, fibers, and waste that is in the colon.
The LBT has also not been validated for use while the subject is eating during the period of time when collecting breath samples. This is no more validated than collecting a blood lipid panel while doing a non-fasting high fat diet. We all understand that the blood lipid panel will be affected by food that was recently ingested.
The LBT was validated to look at hydrogen and methane in the small intestine, which will occur within the first 90 minutes of the test. If a study collects breath samples while eating over a 10-14 hour period and then compares data points, what exactly are they measuring?
The first study – A Low FODMAP Diet Is Associated With Changes In The Microbiota And Reduction In Breath Hydrogen But Not Colonic Volume In Healthy Subjects: healthy subjects ate their habitual diet for 7 days, then provided a stool sample and swallowed transit markers. They were provided a 24 hour standard food package that was not LFD, and then completed a LBT the following morning. They followed a LFD for one week and then were randomized into two groups – the LFD control group was supplemented with maltodextrin. The HFD group was supplemented with oligofructose (prebiotic oligosaccharide, fructans). On the final day of the diet intervention they were provided a standard food pack that was LFD (not the correct LBT diet prep), followed by a LBT the following day. [32]
Concerns with this study:
- The subject pool is healthy subjects – not IBS, nor SIBO.
- Proper food prep and fasting were not performed for the LBT.
- This is not a LFD vs. HFD food intervention. This is an LFD + dextrin vs. LFD + fructans intervention on healthy individuals.
- The differences seen with hydrogen likely represent the differences in colonic fermentation of the standard food packages offered the day before the LBT.
The second study – Randomised Clinical Trial: Gut Microbiome Biomarkers are Associated with Clinical Response to a LFD in Children with Irritable Bowel Syndrome: 33 children with IBS were monitored for 7 days on their habitual diet, they then were randomized into a 48-hour LFD or typical American childhood diet (TACD), followed by a 5 day washout, then crossed over to the other diet intervention for 48 hours. LBT was administered on day two of each intervention diet. Samples were collected for ≥ 8 hours, up to 15 hours, while they ate. [23]
Concerns with this study:
- Proper food prep and fasting was not performed for the LBT.
- They ate during the LBT.
- LBT data was collected and analyzed over a 15 hour timespan.
This study did draw some interesting conclusions: “gas production did not correlate with pain, but may be a potential fermentation marker rather than a direct inducer of symptoms. Change in symptoms is more likely due to reduction in distention, reducing visceral hypersensitivity, than it is to sweeping uniform changes in the microbiota or immune system.”
The third study – one of the most cited studies within the SIBO world – Manipulation Of Dietary Short Chain Carbohydrates Alters The Pattern Of Gas Production And Genesis Of Symptoms In Irritable Bowel Syndrome: 15 healthy subjects and 15 IBS subjects were randomized into two groups. They ate either a LFD (9 grams per day) or HFD (50 grams per day) for two days, followed by a 7 day wash out period, and then crossed over to the other 2 day diet intervention.
Food was provided. From breakfast through lunch the LFD group was offered rice flakes, lactose free milk, tea, rice bread, margarine, orange juice, tea with lactose free milk, an orange, rice pasta with red sauce and lemonade with sugar. [15] Are we to use this menu, which is high in ‘white’ processed food and sugar, as a model to apply the LFD clinically?
Concerns with this study:
- Proper food prep and fasting were not performed for the LBT
- LBT data was collected and analyzed over a 14-hour timespan.
- They ate during the LBT – we cannot then deduce from this data that a LFD or a HFD increases or decreases hydrogen.
- They did not control for the timing of the meals that were consumed across the day. They provided the food and allowed subjects to choose when they would consume these foods across the day. Differences in hydrogen production could be due to timing with meals consumed, or, differences in transit time between the groups.
Though both groups had higher hydrogen levels in response to the HFD, the IBS group had higher levels than the healthy controls. There could be two reasons for this:
The first, this was due to what they were fed (stay with me here – I know that they were measuring diet). The HFD group was given soda with high fructose corn syrup. With IBS, it has been shown that fructose malabsorption alone leads to osmotic diarrhea as well as gas and bloating due to excess fermentation in the colon, [20, 24-27] and not from FODMAPs in general.
Second, the increase in hydrogen could have also been a result of the sorbitol, in the two pieces of chewing gum that they were allowed, in combination with fructose from the HFCS soda. This combination has been shown to exacerbate symptoms by swiftly delivering malabsorbed carbohydrates to the colon, as seen in the study, Fructose-sorbitol ingestion provokes gastrointestinal symptoms in patients with eating disorders. [28]
There was a fourth study that reported a small difference in hydrogen production in response to a LFD, Fodmaps Alter Symptoms and the Metabolome of Patients with IBS: A Randomised Controlled Trial Mcintosh et.al. There was no statistical significance found when comparing baseline data to post diet intervention data. The authors then threw out the baseline data and had to adjust the post diet intervention data to find a statistical significance within groups of patients with IBS. Yet, they didn’t properly food prep their subjects for the LBT and they collected and analyzed LBT data over a 5 hour period. [22]
You Want To Change The Microbiome?
Studies that have investigated microbiota key traits in IBS are able to identify distinct profiles in the intestinal microbiota and organic acids [33], yet the idea that a LFD will directly treat this, is yet to be seen. To date, the LFD has been shown to reduce symptoms, but it has not been shown to directly treat the underlying mechanisms that are at the root of IBS and SIBO.
Strict FODMAP reduction shows unfavorable changes to the microbiota, with little known impact to long term health. A LFD reduces Bifidobacterium [34-36], it reduces beneficial SCFA [37], which could impair the bowel barrier function by leading to the apoptosis of epithelial cells [38,39] and increase in proteolytic fermentation (fermentation of unfavorable BCFA versus SCFA). [40]
We can all agree that altering diet will alter the microbiome in some way. But the idea that we can use a LFD to cherry pick and reduce the specific species that are causing IBS or SIBO is unfounded. Additionally, another study found that the LFD made the microbiota more dysbiotic [18], in a group that has already been shown to have a dysbiotic microbiota. [41] “If dysbiosis is causal in IBS, although there is no direct evidence to support this, then the effect of a strict low-FODMAP diet might be counterproductive.” [42]
Fodmaps Alter Symptoms and the Metabolome of Patients with IBS: A Randomised Controlled Trial Mcintosh et.al.investigated LFD and the microbiome. There was no statistical significance found when comparing baseline data to post diet intervention data. The study states, “… No difference in alpha and beta diversity when comparing baseline samples and post treatment samples.” Yet, the study goes on to compare post intervention data only, making sweeping claims with regard to changes seen with the microbiome, in response to LFD vs. HFD diet. [22]
Two review articles summarized their investigation into IBS and the microbiota:
“… the investigation of the intestinal microbiota in IBS is difficult due to the heterogeneity of this condition, and the effects of an altered intestinal microbiota may not be consistent across all subtypes of IBS (D-IBS, C-IBS and M-IBS).” [43]
Based on the systematic review, “low FODMAPs appear to reduce gastrointestinal symptoms for a least a subset of patients with IBS. However, due to the heterogeneity of reviewed studies, the influence on patients’ gut microbiome composition and/or microbiota metabolites requires additional studies.” [44]
Do You Want to Alter the Immune System?
There is one study that has looked at HFD, lipopolysaccharides (LPS) and visceral hypersensitivity, mainly in rats, but also in 6 IBS-D patients. In 6 of the rats, it was found that fecal LPS was higher in the HFD vs. control diet (8.6 vs 5.1 EU/ mg).
The study claims that a HFD …”induces mucosal inflammation and impaired gut permeability,” yet, as we extrapolate this to humans, this is a stretch. Rat chow, made to mimic a HFD, with lactose, FOS and fructose added, may cause mucosal inflammation and impaired gut permeability in rats placed under one hour of constant stress per day (as they did in this study), but it will never correctly mimic a whole foods diet with altered FODMAP content. The authors do caution “It should be noted that rodent and human microbiota may differ significantly. Hence, caution should be exercised in extrapolating our data to explain human disease.” [45]
What is more of interest are the 6 IBS-D patients – it appears that the researchers preferentially chose their 6 subjects from a group of qualified participants, ‘Human fecal samples were collected from 6 patients showing significant reductions in abdominal symptoms before and following the 4-week LFM diet (LFD).’
Fecal samples were taken from the 6 human subjects, both pre and post-intervention and administered intracolonically into naïve rats. Pre- LFD intervention fecal samples increased visceral hypersensitivity in the rats. Post-diet intervention fecal sample did not increase visceral hypersensitivity.
From these results, should we infer that a person with IBS-D should be placed on a LFD long term? Isn’t it a more plausible conclusion from this 6 person hand selected group, that people with IBS-D and an elevated fecal LPS may benefit from following a 4 week elimination phase LFD and practitioners might consider a LFD as adjunct support, combining this with other clinical interventions that are known to help heal up leaky gut?
Additional studies have shown mixed results
In a mouse study, LFD did not exacerbate nor mitigate inflammation; noting that microbiota profile changes were largely driven by inflammation rather than diet and the LFD caused a shift toward proteolytic fermentation following inflammation. [46]
In a human study, they compared LFD + dextrin vs. LFD + FOS. The LFD showed improvements of symptoms, and a reduction in IL-6 and IL-8, but also a decrease in SCFA and an increase in colonic pH – TNF-alpha were unchanged. [18]
Another human study, Effect of diet and individual dietary guidance on gastrointestinal endocrine cells in patients with irritable bowel syndrome (Review), looked at changes in duodenal enteroendocrine cells in patients with irritable bowel syndrome following a LFD. This review of the original study, by the same author, showed that 3-4 consecutive months on a self-followed LFD, increased serotonin production and the density of somatostatin cells, and quality of life; diarrhea and pain reduced, but constipation did not improve. [47] 46 IBS subjects started this study and only 14 subjects completed it (30% retention rate). This study was characterized by a high dropout rate, which is consistent with previous studies involving IBS patients. [8, 47-50]
In addition to the LFD, the subjects were also instructed to remove corn, legumes, wheat and artificial sweeteners from their diet. They included lactose free dairy products, alcohol and peeled apples and pears (the latter two are high in polyols and traditionally pulled with a LFD).
Is the increase in somatostatin cell density a result of a LFD, and/ or removing gluten, legumes, corn, and artificial sweeteners from the diet? Or, a combination of these AND a shift to whole foods eating; as removing gluten, corn, legumes and artificial sweeteners from a diet would force a shift from packaged foods to whole foods. [47]
Another question to ask – would these results reversed when the LFD is expanded, or when corn and wheat are reintroduced?
In conclusion
Before we continue to perpetuate this wave of fanfare for the LFD, we must first accept that the studies to date have offered mixed results, with the vast majority proving unfavorable. At this time, the LFD has consistently been shown to alter symptoms in some people with IBS.
We need further investigation into the long term effects on the microbiome and immune system. We need studies to implement the LBT in a validated way, so they may correctly interpret the impact of the LFD. “Inconsistencies between studies may be related to differences in habitual diets or differences in sample collection and analysis methodologies. The impact of these changes on gut function and symptoms remains to be elucidated.” [58] The impact on the intestinal microbiota specifically, has to be further investigated, before anyone can ‘safely’ implement a LFD long term.
In, The Pervasive Misunderstanding Of What The Fodmap Diet Does And Does Not Do – Part Two, I discuss the misconceptions around LFD and histamine levels and how this is being incorrectly interpreted across current publications, LFD induced changes in nutrient status, the drawbacks to implementing a sweeping low FODMAP diet protocol clinically, and how to correctly implement the LFD into your clinical practice.






