Mount Sinai scientists have identified primary markers of inflammation IL-6 and TNF-α reliably predict COVID severity and likelihood of survival. This is providing a foundation for a diagnostic platform and therapeutic targets, according to a study published in Nature Medicine.
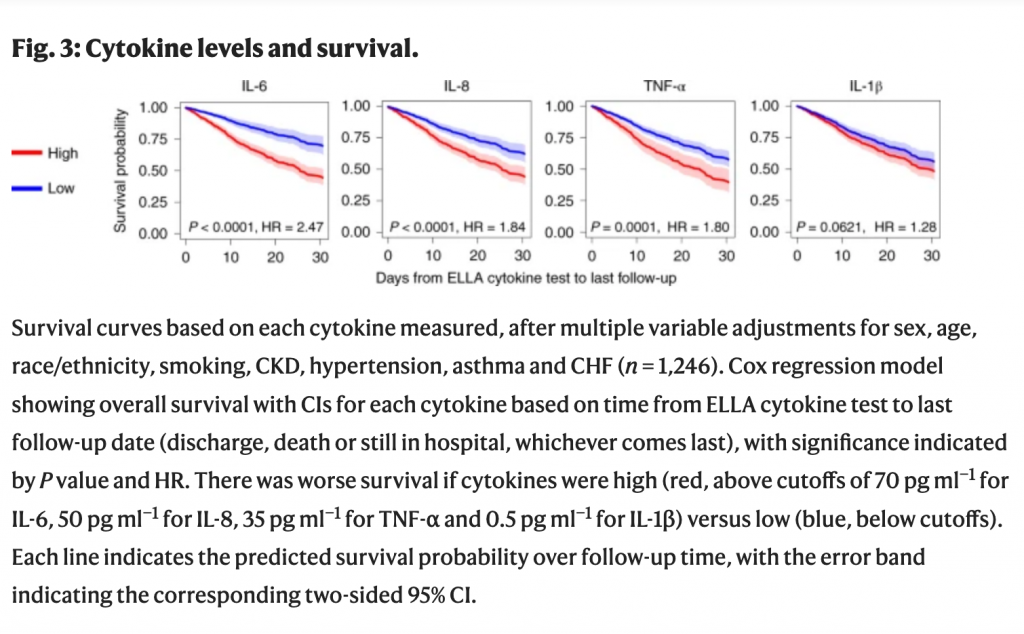
The researchers studied four proteins serum interleukin (IL)-6, IL-8, tumor necrosis factor (TNF)-α and IL-1β, all known as cytokines that circulate in blood and are commonly associated with infections. Researchers found that high serum IL-6, IL-8 and TNF-α levels at the time of hospitalization were strong and independent predictors of patient survival. Two of them, IL-6 and TNF-α, were able to predict which patients were likely to develop more severe forms of COVID-19 and die.
The scientists established that the levels of IL-6 and TNF-α in serum, when measured at admission to the hospital, were elevated in patients who fared the worst, a finding that was independent of the patients’ other underlying medical conditions, of demographics such as age and sex, and of other standard clinical biomarkers of disease severity such as low blood oxygen saturation and common markers related to inflammation, iron levels, and blood clotting issues.
This study suggests that these cytokines should be monitored in the treatment of COVID-19 patients to help select those who should enter clinical trials and receive specific drugs that can target them, the researchers say. Notably, when adjusting for disease severity, common laboratory inflammation markers, hypoxia and other vitals, demographics, and a range of comorbidities, IL-6 and TNF-α serum levels remained independent and significant predictors of disease severity and death.
“We propose that serum IL-6 and TNF-α levels should be considered in the management and treatment of COVID-19 patients to stratify prospective clinical trials, guide resource allocation, and inform therapeutic options,” said lead researcher Sacha Gnjatic, PhD, Associate Director of the Human Immune Monitoring Center at Mount Sinai; Associate Professor of Medicine, Oncological Sciences and Pathology, at the Icahn School of Medicine at Mount Sinai; and a member of the Precision Immunology Institute and The Tisch Cancer Institute at Mount Sinai.
“We also propose that patients with high IL-6 and TNF-α levels should be assessed for combinatorial blockade of pathogenic inflammation in this disease. Drugs blocking these cytokines are either FDA-approved or in clinical trials.”
When the pandemic began, Mount Sinai scientists promptly implemented a rapid test to measure the levels of four cytokines associated with pathogenic inflammation, which were suspected to cause severity in COVID-19 patients. In just one month, cytokine blood levels were tested in 1,484 patients upon admission to Mount Sinai Health System’s hospitals, and patients were followed for up to 41 days.
Thanks to an emergency authorization from the New York State Department of Health, the test was allowed to be placed in the hospital’s electronic medical record system where doctors order standard blood tests and medicines for patients, allowing for the rapid collection of a large amount of samples. Results were available in three hours, leading researchers to believe it could be implemented in a clinical setting to stratify patients and determine treatments in almost real time.
The results from the tests showed that the risk of death in patients with elevated IL-6 or TNF-α was twofold or higher, even when considering other known risk factors. Scientists then validated their predictive model using samples from an additional cohort of 231 hospitalized COVID-19 patients.
The researchers looked at how various treatments attempted in a subset of these patients affected the cytokines they measured. They found that treatments recently found to benefit COVID-19 patients, such as the antiviral remdesivir or the corticosteroid dexamethasone, could lower the levels of the cytokines.
The researchers note that although the data do not demonstrate a causative role for IL-6 and TNF-α in disease outcome, they did record the effects of various treatments on measured cytokines. This serves as potential mitigation strategies should there be a pathogenic effect from these inflammatory agents. Here is what they found:
- From a subset of 244 patients with more than one ELLA cytokine assay performed, and by mapping time from treatment start to first ELLA test, they were able to assess the effects of various treatments and experimental drugs on cytokine levels (Fig. 5a).
- The analysis of a subset of patients with progressive respiratory failure and marked systemic inflammation who received off-label treatment with the anti-IL-6 receptor monoclonal antibody tocilizumab showed that these patients started with elevated IL-6 levels and then had a transient increase in serum IL-6, which has previously been explained by disrupted clearance after drug saturation of the IL-6 receptor21.
- This transient elevation was observed only for IL-6, not IL-8, whereas TNF-α appeared to gradually decrease after therapy.
- Patients treated with corticosteroids and remdesivir showed, respectively, a rapid and gradual reduction in IL-6 over time compared to patients who did not receive these drugs, but we observed no effect on TNF-α.
- Hydroxychloroquine, acetaminophen or anti-coagulants did not clearly appear to alter cytokine levels. Of corticosteroids, dexamethasone had the highest reduction effect on IL-6 (Fig. 5b), potentially supporting findings from the recent RECOVERY trial showing clinical benefit from this drug in hospitalized patients with severe disease
Based on these results, scientists propose that monitoring COVID-19 patients for these cytokines can help determine their prognosis, and that any treatment should be potentially administered in the context of cytokine measurements, since it affects outcome. The researchers propose that these findings also call for the use of drugs targeting IL-6 and TNF-α by themselves or combined at the same time, to be tested for their potential benefit based on elevated starting levels.
Conclusion/ Monitoring the levels of IL-6 and TNF-a before and during experimental treatments such as anti-cytokine antibodies or corticosteroids will be useful to establish a predictive and prognostic value for these potential biomarkers.
Editor’s Note: This study falls in line with previous work by integrative practitioners Joe Pizzorno, ND, IMCJ editor-in-chief and co-authors, Sam Yanuck, DC and, Helen Messier, MD, PhD, Kara Fitzgerald, ND on a phased approach to COVID-19. Read more here.
Click Here for Full Text Study