Research in past decade shows that iron, from food and supplementation, may increase the risk of premature age-related macular degeneration. A recent study, published in Retina, outlines the importance of discussing this risk for patients who may be taking iron unknowingly – in a multi-vitamin or by self-indication – and not know how this could raise their risk of AMD.
Today’s Practitioner consulted with Mary Louder, DO to get her thoughts on the  importance of prescribing heavy metal chelation for cases outlined in this study. At the bottom of this post, we offer a video from Age-Related Eye Disease Study (AREDS 2) from Kimberly Reed, OD, FACM, sponsored by Optometry Today. Dr. Reed calls the negative medical media response to AREDS2 a tragedy, adding that there is much we can still learn about this study in regard to supplements and eye health.
importance of prescribing heavy metal chelation for cases outlined in this study. At the bottom of this post, we offer a video from Age-Related Eye Disease Study (AREDS 2) from Kimberly Reed, OD, FACM, sponsored by Optometry Today. Dr. Reed calls the negative medical media response to AREDS2 a tragedy, adding that there is much we can still learn about this study in regard to supplements and eye health.
Abstract / Because patients often take iron supplements without medical indication, and iron can accumulate in vascular endothelial cells, the authors evaluated the association of oral iron supplementation with retinal/subretinal hemorrhage in patients with neovascular age-related macular degeneration.
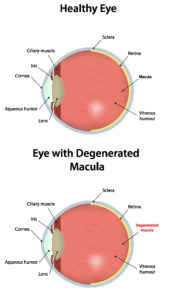
Many patients have taken steps to add iron to their supplements, usually through a multi-vitamin with iron. When this is encountered, I am concerned because iron being a heavy metal can promote oxidative damage when deposited in various locations in the body,” says Dr. Mary Louder. Macular degeneration has a known consideration for oxidative damage on the macula which promotes the proliferation of drusen. Iron and other heavy metals can be implicated in this.”
In this study, a post hoc secondary data analysis of comparison of age-related macular degeneration treatments trials was performed. Participants were interviewed for use of oral iron supplements. Trained readers evaluated retinal/subretinal hemorrhage in baseline fundus photographs. Adjusted odds ratios from multivariate logistic regression models assessed the association between iron use and baseline hemorrhage adjusted by age, sex, smoking, hypertension, anemia, and use of antiplatelet/anticoagulant drugs.
Results / The following outlines the results among the 1,165 participants:
- Baseline retinal/subretinal hemorrhage was present in the study eye in 71% of 181 iron users and,
- In 61% of 984 participants without iron use (adjusted odds ratio = 1.47, P = 0.04), and the association was dose dependent (adjusted linear trend P = 0.048). Iron use was associated with hemorrhage in participants with hypertension (adjusted odds ratio = 1.87, P = 0.006) but not without hypertension. The association of iron use with hemorrhage remained significant among hypertensive participants without anemia (adjusted odds ratio = 1.85, P = 0.02).
- Among participants of comparison of age-related macular degeneration treatments trials, the use of oral iron supplements was associated with retinal/subretinal hemorrhage in a dose-response manner.
- Unindicated iron supplementation may be detrimental in patients with wet age-related macular degeneration.
For the reasons stated above, Dr. Louder frequently tests patients for heavy metals because many may not realize they’ve come in contact with excess iron or other metals.
A review of the literature indicates that chelation is the most effective way to remove metals and in this case iron stores for the body,” she says. “I see effective treatments with IV EDTA chelation and other measures to decrease oxidative damage and stress as well as inflammation. There may be an indication for elective phlebotomy due to elevated hemoglobin, hematocrit and elevated iron levels such as in hemochromatosis. If these blood tests are normal, or if there is an iron storage disease then EDTA chelation is effective.” The key to remember is that wherever there are heavy metals, oxidative damage is soon to follow.
Conclusion / The use of oral iron supplements was associated with retinal or subretinal hemorrhage in a dose-dependent manner among the 1165 participants (aOR, 1.47; P=.04). Increased iron intake may be associated with higher rates of hemorrhage in the setting of wet neovascular AMD; therefore, it is recommended that these patients consult with their ophthalmologists before initiating any supplementation or medication that has not been prescribed.
Above all, this study points to the importance of nutrition counseling and eye health. This video from Optometry Today reviews the literature concerning nutrition and supplements with respect to ocular disease and examines the literature in the context of clinical practice. This video includes a discussion of AREDS and AREDS 2 and a critical evaluation that you may not have seen about the role of omega-3 fatty acids, carotenoids, vitamins and trace minerals in ocular disease.
Source: D Song, DF Martin et al. Association Between Oral Iron Supplementation and Retinal or Subretinal Hemorrhage in the Comparison of Age-Related Macular Degeneration Treatments Trials. Retina (Philadelphia, Pa.) 2018 Aug 28;[EPub Ahead of Print].