Have you ever noticed your patients’ decision patterns when opting for integrative and complementary health  approaches (ICHA) to specific health issues? This latest study, published in BMC Complementary and Alternative Medicine, shows how and why people may prefer ICHA in some situations and but not in others. These choices largely depend on the characteristics of the illness to face. This study examined distinct patterns of attitudes toward ICHA in people hypothetically facing chronic illnesses and differed by severity and clinical expression. These findings may help you better understand whether patients will opt for ICHA, either in addition to (i.e., complementary attitude) or in place of (i.e., alternative attitude).
approaches (ICHA) to specific health issues? This latest study, published in BMC Complementary and Alternative Medicine, shows how and why people may prefer ICHA in some situations and but not in others. These choices largely depend on the characteristics of the illness to face. This study examined distinct patterns of attitudes toward ICHA in people hypothetically facing chronic illnesses and differed by severity and clinical expression. These findings may help you better understand whether patients will opt for ICHA, either in addition to (i.e., complementary attitude) or in place of (i.e., alternative attitude).
In this study, complementary and alternative attitudes toward ICHA were examined in people hypothetically facing chronic illnesses that differed according to their severity and clinical expression.
Study Parameters
The web-based study included 1807 German participants. They were asked to imagine that they had a particular chronic illness based on clinical vignettes: depression, schizophrenia, and somatic illnesses, such as rheumatoid arthritis, multiple sclerosis. Participants were invited to rate their perceived distress and social stigma associated with each illness as well as its perceived treatments. They also rated their belief in treatment effectiveness, and their treatment preference. Four patterns of treatment choice were determined: strictly conventional, weak or strong complementary, and alternative.
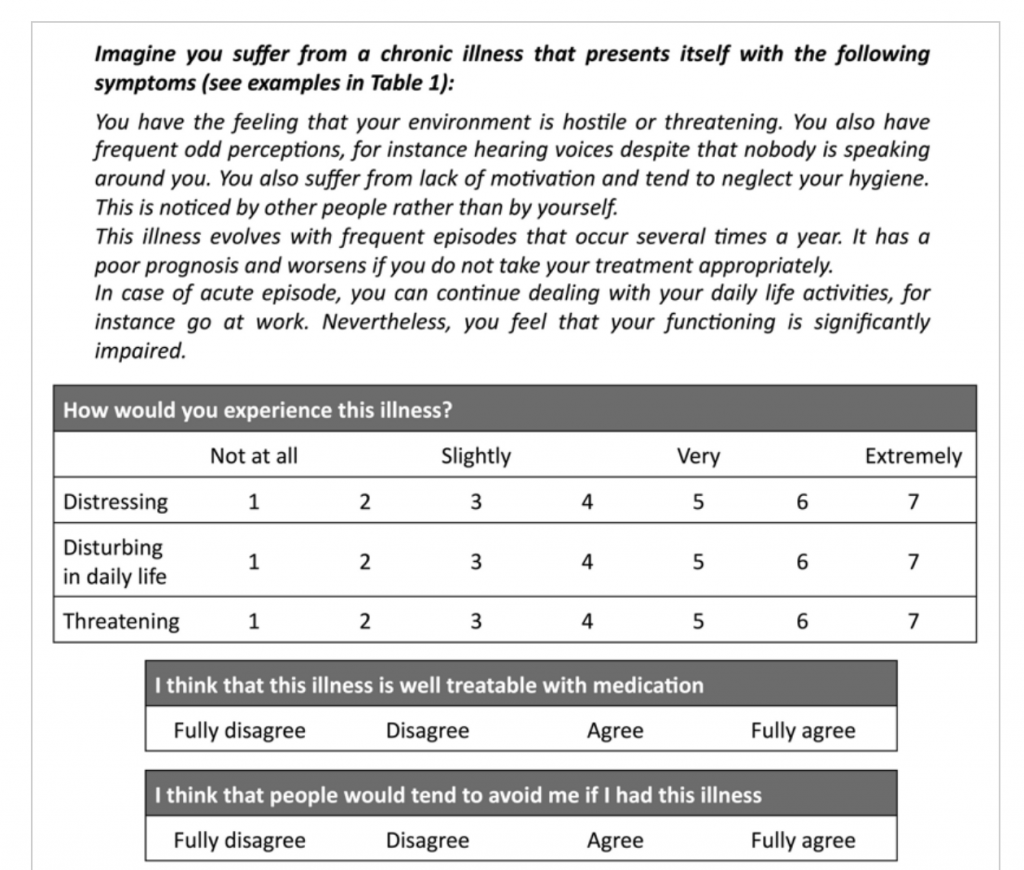
Here are examples of clinical vignettes offered to study participants, with levels of severity and relapse frequency:
Schizophrenia: “You have the feeling that your environment is hostile or threatening. You also have frequent odd perceptions, for instance hearing voices, despite that nobody is speaking around you. You also suffer from lack of motivation and tend to neglect your hygiene. This is noticed by other people rather than by yourself.”
Recurrent Depression: ““You experience a groundless sadness and lose your joy of life. You also notice that you lack motivation or inner impulse for your daily life activities. Your capacities to concentrate are considerably reduced (for instance when reading or watching TV).”
Multiple Sclerosis: “You suffer from a lack of (muscular) strength in your legs. This weakness waxes and wanes from day to day and is unpredictable. You also have deficits in sensitivity in particular parts of your body and you suffer from enduring impaired vision.”
Rheumatoid Arthritis: “You suffer from pain in yours joints, particularly in your knees, elbows, hands and fingers, which you feel more or less constantly. These pains are disturbing in your daily life and also at night.”
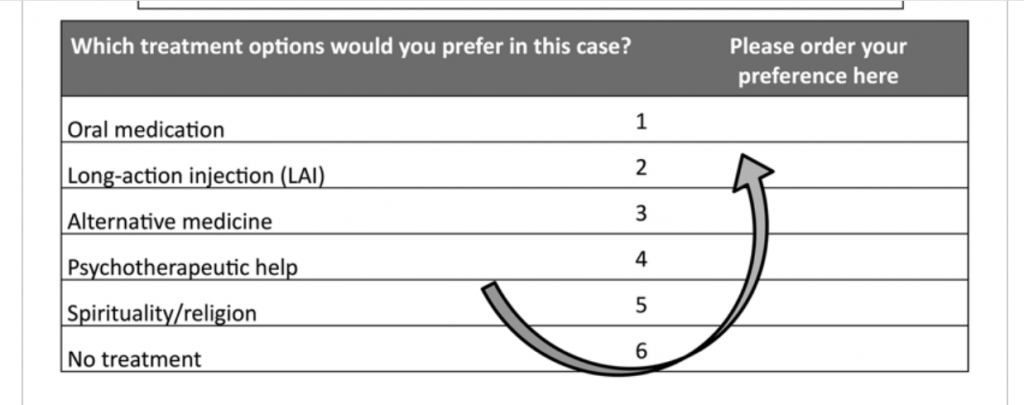
From here, participants complete questions to assess their belief in the effectiveness of each of the treatment options. Then, for each illness, participants were invited to rate on a 4-point scale (1 = fully disagree, 2 = rather disagree, 3 = rather agree, 4 = fully agree) the following statement: “I consider the following treatment option as efficient for schizophrenia (or RD, MS, RA)” followed by each treatment option. This provided researchers with a “score of belief in treatment effectiveness.”
For each clinical vignette, treatment choices were categorized in four patterns of choice:
1. “Strictly conventional” for people selecting pill, LAI or psychotherapy as unique treatment option excluding ICHA or spiritual guidance.
2. “Weak complementary” for people selecting pill or LAI as first treatment option combined with ICHA as further treatment option.
3. “Strong complementary” for people selecting ICHA or spiritual guidance as first treatment option combined with conventional treatment as further treatment option.
4. “Alternative” for people selecting ICHA or spiritual guidance as unique treatment option, excluding conventional treatment options (pill, LAI or psychotherapy).
Results
- People hypothetically facing chronic illnesses selected ICHA as complementary treatment option in a large majority of cases, and only 4.8% (43/899) selected strictly conventional medicine (i.e., excluding ICHA) as unique treatment option.
- ICHA were mostly selected as secondary treatment option in addition to conventional medicine. The second most preferred treatment option placed ICHA before conventional medicine.
- All in all, the complementary attitude towards ICHA was largely predominant (41.1% of people selecting it as unique treatment option and 94.2%selecting this option at least once), whereas the alternative attitude was rarer (2.1% of people selecting it as unique treatment and 25.9% selecting this option at least once).
- 65 participants (11.2%) compared to 49 (8.3%) selected the strictly conventional option as single treatment option for mental and somatic illnesses, respectively, and 30 participants (5.2%) compared to 15 (2.7%) selected the alternative option as single treatment option for mental or somatic illnesses, respectively.
- In total, 106 participants (30 + 76, 11.8%) selected at least once the alternative option for mental illnesses compared to 82 participants (15 + 67, 9.1%).
- The results are in line with previous studies showing that more than 80% of patients with cancer use ICHA in addition to chemotherapy during the beginning of cancer treatment, indicating that patients facing severe illnesses often use ICHA as complementary treatment in the early phase of their illness.
The study revealed that the propensity to use ICHA is not a stable and fixed characteristic of individuals but varies according to the characteristic of the illness.
In fact, 421 participants (46.8%) exhibited the same pattern of treatment preference whatever the descriptions of the clinical vignettes, while the other part of the sample (478 participants, 53.2%) adapted their choice and showed a flexible patterns of treatment preference.
Conclusion/ From the point of view of scientific medicine one may expect that people facing severe illnesses would mainly select conventional and evidenced-based treatments. This study provides new evidence that for both mental and somatic illnesses, medical pluralism is the norm, that is, the integration of complementary medicine in addition to conventional treatment, mostly as second line (but sometimes also as first line) treatment option. Bearing in mind the limitations due to the virtual nature of this study, our results highlight the need to take attitudes toward ICHA into account for a better understanding of patients’ preferences to use ICHA.