Lipoprotein(a), abbreviated as LP(a), is a unique lipoprotein particle that has garnered increasing attention in recent years due to its significant role in cardiovascular health. As an emerging biomarker, LP(a) is now recognized as a crucial factor in assessing a patient’s risk for atherosclerosis, coronary artery disease (CAD), and other cardiovascular conditions. This article provides an in-depth exploration of LP(a), the clinical importance of its measurement, and the follow-up evaluations and interventions warranted for patients with elevated levels.
What is Lipoprotein(a)?
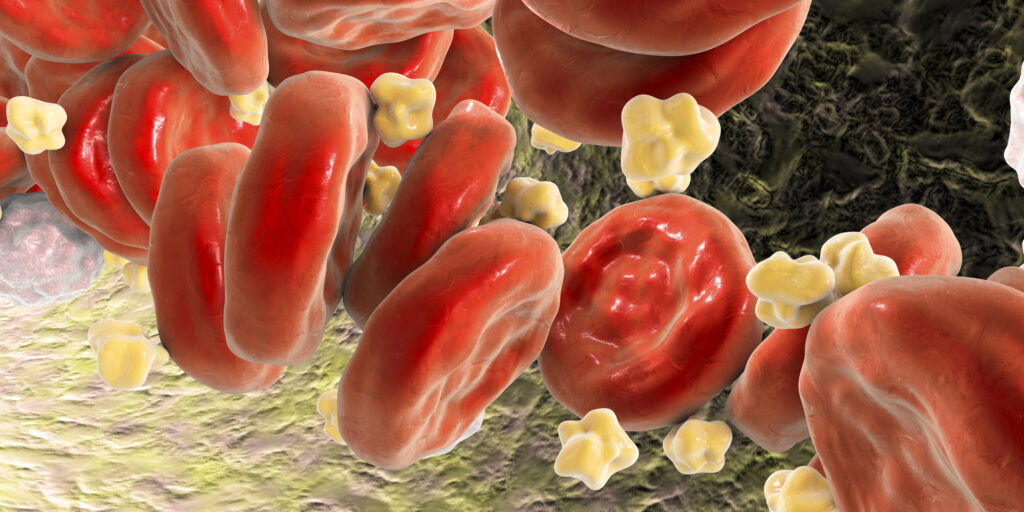
Lipoprotein(a) is a lipoprotein subclass that consists of an LDL-like particle bound to a large glycoprotein known as apolipoprotein(a). Structurally, it resembles low-density lipoprotein (LDL) but differs due to the presence of apolipoprotein(a), which imparts unique functional and pathological properties. Elevated LP(a) levels are primarily determined genetically, with little influence from diet, exercise, or standard lipid-lowering therapies.ⁱ Its clinical significance lies in its pro-atherogenic, pro-inflammatory, and pro-thrombotic properties.
Why is the LP(a) Test Important?
Testing for LP(a) provides critical information about cardiovascular risk that is independent of traditional lipid profile metrics. Elevated LP(a) levels have been associated with the following:
- Atherosclerosis: LP(a) contributes to the development of plaques within arterial walls by promoting cholesterol deposition and inflammation.
- Thrombosis: Its structural similarity to plasminogen interferes with fibrinolysis, increasing clot formation and the risk of thrombotic events.
- Early-Onset Cardiovascular Disease (CVD): Patients with high LP(a) are at a markedly increased risk of premature CAD, stroke, and myocardial infarction.
- Residual Risk in Statin Therapy: For patients whose LDL-C levels are well-controlled with statins, elevated LP(a) may account for residual cardiovascular risk.
Ideal Range and Clinical Interpretation
LP(a) levels are typically measured in milligrams per deciliter (mg/dL) or nanomoles per liter (nmol/L). While there is no universal consensus on the ideal range, the following thresholds are commonly used:
- Low Risk: <30 mg/dL (<75 nmol/L)
- Intermediate Risk: 30-50 mg/dL (75-125 nmol/L)
- High Risk: >50 mg/dL (>125 nmol/L)
Elevated LP(a) levels, particularly above 50 mg/dL, are associated with a two- to fourfold increased risk of cardiovascular events.
Additional Tests for Patients with Elevated LP(a)
For patients whose LP(a) levels are above the ideal range, further diagnostic evaluations are essential to stratify risk and guide management. Recommended tests include:
- Advanced Lipid Panel:
- LDL particle size and number
- Non-HDL cholesterol
- Imaging Studies:
- Coronary Artery Calcium (CAC) Scoring: Evaluates the extent of calcified plaque in coronary arteries.
- Carotid Intima-Media Thickness (CIMT): Measures subclinical atherosclerosis.
- Inflammatory Biomarkers:
- High-sensitivity C-reactive protein (hs-CRP): Assesses systemic inflammation.
- Fibrinogen levels: Reflect thrombotic risk.
- Genetic Testing:
- Identifies familial hyperlipidemias and other genetic conditions that may coexist with elevated LP(a).
- Coagulation Studies:
- Assess thrombotic risk through tests like D-dimer, Factor V Leiden mutation, or prothrombin gene mutation analysis.
- Functional Cardiovascular Assessments:
- Stress testing or coronary angiography for symptomatic patients or those with high-risk profiles.
Treatment and Management Options
Currently, there are no FDA-approved therapies specifically targeting LP(a) reduction, as stated in the 2018 AHA/ACC Guidelines for the Management of Blood Cholesterol. However, various strategies can mitigate its associated cardiovascular risks:
- Lifestyle Modifications:
- Although LP(a) is largely genetic, maintaining a healthy diet, regular exercise, and smoking cessation can reduce overall cardiovascular risk.
- Pharmacologic Therapies:
- PCSK9 Inhibitors: Shown to reduce LP(a) levels by up to 30% in addition to LDL-C.
- Niacin: Historically used to lower LP(a), though its routine use is controversial due to limited outcome data.
- Aspirin: Considered for its antithrombotic effects in select patients.
- Emerging Therapies:
- Antisense Oligonucleotides (ASOs): Under investigation, ASOs like pelacarsen specifically target apolipoprotein(a) production, significantly lowering LP(a) levels.
- Risk-Based Interventions:
- Aggressive management of other modifiable cardiovascular risk factors, such as hypertension, diabetes, and dyslipidemia.
- Intensified statin therapy to lower overall LDL-C, despite no direct impact on LP(a).
Conclusion
LP(a) is a powerful biomarker that enhances the clinician’s ability to identify patients at heightened cardiovascular risk. Elevated levels warrant a comprehensive assessment, including advanced imaging, genetic evaluations, and inflammatory markers, to tailor preventive and therapeutic strategies effectively. With ongoing advancements in targeted therapies, the future holds promise for more robust management of LP(a)-related risks. Recent studies, such as those on pelacarsen, highlight the potential of emerging treatments to significantly reduce LP(a) levels and associated risks. Awareness and understanding of LP(a) among medical professionals are critical for optimizing patient outcomes and mitigating the burden of cardiovascular disease.
References
- Tsimikas, S. “A Test in Context: Lipoprotein(a): Diagnosis, Prognosis, Controversies, and Emerging Therapies.” Journal of the American College of Cardiology, 2017.
- Nordestgaard, B. G., et al. “Lipoprotein(a) as a cardiovascular risk factor: Current status.” European Heart Journal, 2010.
- Kamstrup, P. R., et al. “Lipoprotein(a) and risk of myocardial infarction—genetic epidemiology.” Arteriosclerosis, Thrombosis, and Vascular Biology, 2009.
- Emerging therapies for LP(a): Clinical Trials Overview—Pelacarsen and Beyond. Current Cardiovascular Reports, 2023.
- Grundy, S. M., et al. “2018 AHA/ACC Guidelines for the Management of Blood Cholesterol.” Circulation, 2019.