Of the many advances in modern medicine, few are as exciting and promising as those in the field of genetics and genomics. Emerging technology and understanding of genetic influences have the potential to transform health care, allowing for more precise diagnoses, earlier intervention and dramatically improved outcomes for patients.
Genetics and genomics have been used for decades in conventional medicine to identify genetic mutations or variations, determine disease risk, direct the development of pharmaceuticals and guide individual drug treatments. With recent breakthroughs in research and technology, genetics and genomics, genetic testing has become increasingly sophisticated and widespread. Some of the most common applications:
- Diagnosing specific genetic disorders. Single-gene mutations that cause disorders like Huntington’s disease, sickle cell anemia and cystic fibrosis can be detected through genetic testing, as can chromosomal abnormalities linked with Down syndrome, copy number variations associated with autism and schizophrenia, and mitochondrial DNA mutations.
- Identifying heightened risk for disease. Testing can point out genetic mutations or variations that increase the likelihood of developing hereditary cancers, neurological disorders, cardiovascular disease and certain inherited metabolic conditions.
- Improving treatment outcomes for drug therapies. Pharmacogenetics and pharmacogenomics help predict a patient’s response to a drug, to reduce the risk of adverse reactions, inform optimal dosing and increase successful outcomes.
- Addressing chronic pain and pain management. Genes that influence the metabolism of opioids can increase the potential for respiratory depression or overdose. Pharmacogenetic testing is especially useful in long-term pain management to identify patients at a higher risk for opioid addiction.
Most compelling are the possibilities for personalized medicine. Genetic testing allows practitioners to craft customized protocols for early intervention and proactive prevention, tailored to an individual’s specific genetic makeup.
“Our genes are our unique blueprint,” says Amanda Archibald, RD, founder and principal, The Genomic Kitchen. “Having that blueprint for a patient helps us direct efficient care and create cost-effective, useful and informed outcomes. When you start with genetic input as a foundation for thinking, you’re already ten steps ahead in removing some of the guesswork.”
Unlike imaging, lab work or other diagnostic modalities, genetic testing yields more comprehensive information, revealing subtle clues that might not otherwise be apparent. For example, certain conditions—like autoimmune diseases, hormonal disorders or neurological disorders—are difficult to diagnose with blood work alone. A patient’s genetic profile can offer valuable details to lead practitioners toward underlying points of origin.
“Due to the blood-brain barrier, there’s a lot of information you cannot get from blood work about brain inflammation, brain serotonin levels, brain cortisol levels,” says Sharon Hausman-Cohen, MD, Chief Medical Officer of IntellxxDNA. “But if you know the person has a gene that’s associated with higher brain cortisol production and three times the risk of depression, you can go right to ways to lower their cortisol. Genetic information provides a more accurate map and a targeted starting point.”
Understanding individual genetic influences also offers insights that guide practitioners toward efficient, personalized treatments. Knowing a patient has mutations in the BRCA-1 and BRCA-2 genes, linked with a higher risk of breast and ovarian cancers, or other mutations that increase the likelihood of colon, endometrial and other cancers, allows for early intervention with customized protocols.
Of course, not all patients with a genetic predisposition will develop a disease. Actual risk is greatly impacted by diet, lifestyle and other environmental factors, and genetics helps practitioners identify unique patterns in how an individual reacts to external input.
“Genetic testing answers the question why,” says Yael Joffe, PhD, founder and Chief Science Officer of 3X4 Genetics. “Why do I respond to the world around me in a certain way? If I’m exposed to molds or toxins, if I’m immersed in pollution, I may get ill, and you may be completely fine. Whether we’re talking about why some people develop cancer and others don’t, or why childhood trauma or emotional stressors shut some people down while others are fine, genetics answers the question of why we respond to the world around us in a different way.”
Knowing an individual’s genetic makeup also allows practitioners to monitor disease progression and treatment response over time, adjusting and refining protocols based on clues that other testing modalities can’t provide. Most important, it encourages a uniquely human connection, a deeply personalized way to enlighten and validate patients.
“Genetic testing allows us to look in places far removed from the actual issue,” Archibald says. “It helps us look in dusty corners, under the hood, behind the cobwebs to find out where the inefficiency is that’s actually creating the symptoms or complexity or pain a patient is experiencing. It lets us to put together a thought process, so the patient feels heard, confident and empowered.”
Seven ways genetics and genomics can support your personalized practice.
1. Effective protocols for complex neurodegenerative diseases. Alzheimer’s, Parkinson’s disease, Huntington’s disease and other neurodegenerative disorders are multifaceted and notoriously difficult to treat. Genetic testing can identify contributing factors and inform effective, comprehensive protocols.
“People think about APOE4 as increasing the risk of dementia,” says Hausman-Cohen. “But if you only know APOE4 status, you’re giving the patient incomplete information. We know from studies that only about 20 percent of people who have APOE4 go on to develop dementia. The question is why?”
Genetics and genomics research show many genes interact in the development of dementia—for example, genes that relate to inflammation can influence APOE4, as can hormone receptor gene variants or gene variants involved in detox pathways, she says.
“What about the 35 to 60 percent of people with Alzheimer’s who don’t have APOE4?” says Hausman-Cohen. “Genomics is incredibly helpful in getting those patients well. We look at SNPs that relate to growth factors, brain ischemia, the gut, copper and zinc processing, inflammation, detox, methylation and homocysteine. A lot of people have other triggers for dementia. Maybe they aren’t getting enough oxygen to the brain because their blood vessels are not making enough nitric oxide, or they make too many clotting factors. APOE4 isn’t even close to a complete answer. It doesn’t give patients enough information to help them truly optimize their cognition.”
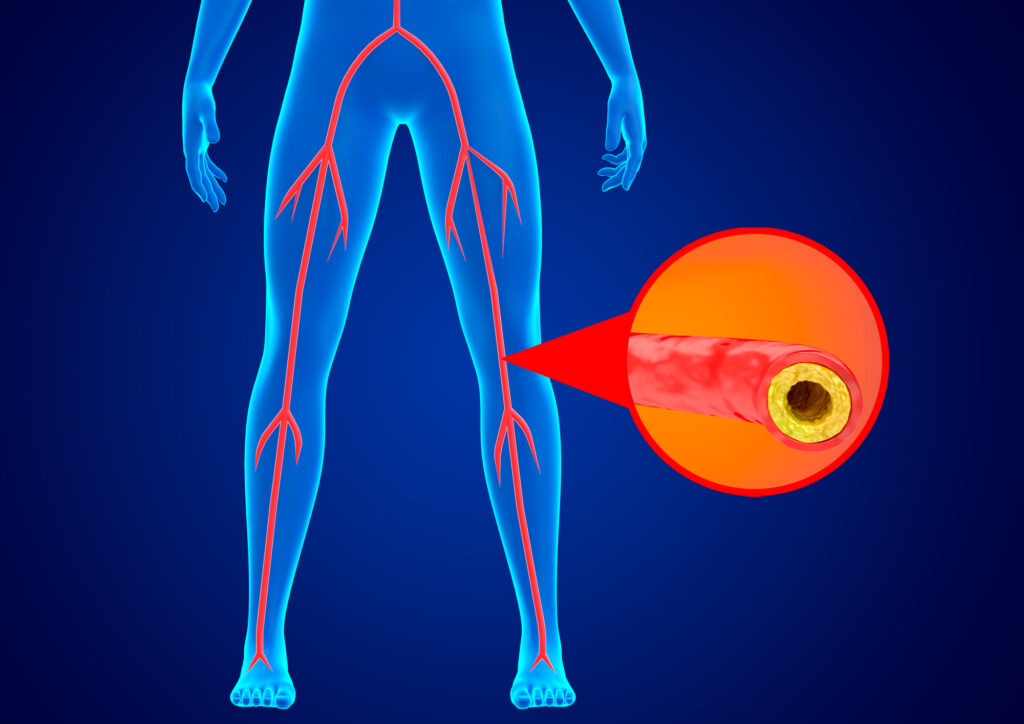
2. Targeted interventions to prevent or treat chronic disease. Heart disease, stroke, diabetes, cancer and other chronic diseases are complex conditions that impact multiple systems. Genetics provides critical data to lead practitioners toward strategic, effective interventions.
“Many clients we’re seeing now have a lot of complex issues,” Archibald says. “There’s no one care plan for any one given system. There are ideas and guidelines, but genetics offers more specific, efficient solutions to address, for example, high blood pressure or heart disease. Maybe this individual has significant oxidative stress potential, or they aren’t detoxifying. If we don’t take care of cellular issues or immune-related issues or absorption issues, it doesn’t matter how we treat high blood pressure. We’re still putting a Band-Aid on something that may have its origins in another system, one we may be able to see through genomic information.”
If a practitioner is addressing cardiometabolic conditions, for example, the first tendency might be to manipulate carbohydrates, or use medications to get blood sugar under control or lower inflammation. “But what if one of the root causes for this patient is immune dysregulation, or a vicious cycle of inflammatory response or autoimmunity that’s driving reactive oxygen species which is driving inflammation?” says Archibald. “With genomics, we can see where the starting point is. It’s an ignition switch to spark thinking about root causes might be, what are the priorities, what do I need to address first as foundational intervention to guide the body back to homeostasis.”
3. Comprehensive plans for obesity and weight management. One of the most perplexing and frustrating issues practitioners face: helping patients lose or maintain weight. Like Alzheimer’s or chronic diseases, weight management and obesity are complex, influenced by a range of factors.
“A patient will come to me and say, ‘I can’t lose weight, I’ve tried everything,'” says Joffe. “So, we’ll do a genetic test and see what comes back. Maybe it’s because their genes that switch on appetite or hunger are stronger than others, maybe that person’s body stores fat really well. Or maybe I’m not seeing anything in the genes that would make a patient gain weight. But if we use an upstream approach, we can find the root cause. We might see where cellular function, inflammation or detoxification is being impacted by genes. So instead of diet or exercise, a practitioner might prioritize reducing inflammation. For that patient, it’s not about calories.”
Even more important, genetic testing confirms and validates an individual’s struggles to lose or maintain weight. “It offers answers for the patient and takes away the shame, the idea that they don’t have any willpower,” Archibald says. “It’s a game changer that allows science to meet empathy and realistic goals and expectations.”
4. Tailored treatment plans for mental wellness. Depression, anxiety, PTSD and other mental health conditions are complex and greatly influenced by a multitude of diverse factors. A patient’s genetic profile can lead practitioners underlying issues and more effective interventions.
“In a meta-analysis published in 2022, the serotonin theory of depression was debunked—something functional medicine doctors already knew,” says Hausman-Cohen. “You can’t just assume depression means someone is low on serotonin. Serotonin isn’t the only cause, and it’s almost never the sole cause. There are so many contributing factors.”
Other neurotransmitters like GABA, cortisol, or dopamine impact mental wellness, she says, as do inflammation, oxidative stress, cortisol levels, and thyroid levels in the brain. If a patient has gene variants that increase the risk for celiac disease, gluten can exacerbate mood symptoms. Homocysteine levels and genes that affect homocysteine also play a key role, along with cofactors involved in neurotransmitter synthesis and function.
“Research shows only 35 percent of people treated with SSRIs at two months were fully well and in remission,” says Hausman-Cohen. “Why? Because you’re missing so many of the root causes. Genomics helps us pinpoint and address these.”
5. Customized diet and lifestyle regimens. Some recommendations, like eliminating sugar or exercising more, will benefit most people. But a cookie-cutter approach seldom works for long—knowing a patient’s genetic profile allows for personalized diet and lifestyle plans that lead to better outcomes.
“We shouldn’t be having any conversation around nutrition without considering an individual’s genetics,” says Joffe. “It’s like trying to create an effective protocol with only 50 percent of the information you need.”
For example, while the DASH diet is routinely recommended for the management of hypertension, “it’s nonsense to say everyone should be on a low-sodium diet to reduce blood pressure,” she says. “For many people, salt has no impact on blood pressure. Multiple genes contribute to whether any one person will develop high blood pressure. Several genetic pathways are implicated in hypertension, including those related to vasoconstriction, dilation, glucose and insulin metabolism, vascular health and nitric oxide production. Without addressing these, you’re not solving the problem.”
Genetic information also allows practitioners to recommend lifestyle interventions in an efficient, directed way. While exercise is generally beneficial for everyone, genetics can inform which approaches are most effective, says Hausman-Cohen. For example, research links high BDNF with significantly slower cognitive decline, she says. If a patient genetically does not make the mature form of BDNF, intense, aerobic exercise—shown to convert the immature form of BDNF to the mature form—becomes ten times more important.
6. Targeted, highly specific supplement protocols. Like diet and lifestyle, supplement regimens aren’t one-size-fits-all. Genetic information helps practitioners develop personalized plans tailored to individual patients.
“Using genomics, we can get much more specific with supplements,” says Hausman-Cohen. “We might say ‘inflammation increases the risk of cognitive decline.’ But that’s too broad. That’s like saying ‘antibiotics kill bacteria.’ What antibiotics? What bacteria? You have to choose anti-inflammatories based on what kind of genomics and what kind of inflammation the person has.”
For example, some of the main types of inflammation associated with cognitive decline are TNF-a, IL-1 alpha, IL-1 beta, CRP and IL-6. “If you know a patient has the TNF-a SNPs linked with cognitive decline, you’re going to want to use the anti-inflammatories that best lower TNF-a and cross into the brain, such as lion’s mane or aloe polymannose complex,” she says “If a patient has cognitive decline because they have IL6 issues, you need something different—omega-3s, quercetin and sulforaphane have been shown to lower IL6 and help cognitive decline.”
7. More successful outcomes, with minimal trial and error. Genetic testing can provide crucial information about a patient’s unique makeup, allowing practitioners to identify underlying causes and focus on the most effective and efficient interventions.
“A trial-and-error approach is costly, in terms of time and money,” says Joffe. “More dangerous is the incredibly high psychological cost. A patient may be desperate to change. We might try something for three weeks. That doesn’t work, so we try something else, and then that doesn’t work. Every time a treatment fails, they feel more and more hopeless and devastated.”
Knowing a patient’s genetic profile can reveal root causes, direct practitioners to targeted interventions that minimize trial and error. “Genetics helps us shorten treatment time and get a successful outcome so much faster,” says Joffe. “Trying to solve a complex condition without genetic data is like having one arm tied behind your back. Without genetics, we’re missing valuable information about our patients and how they respond to the world around them.”