In the early 20th century, several isolated studies discovered a relationship between a person’s diet and mental health. Over one hundred years later, it’s increasingly accepted that the beneficial bacteria and other microorganisms living in our bodies are a crucial link between our diet and mental health by influencing the gut-brain axis.
What is the Gut-Brain Axis?
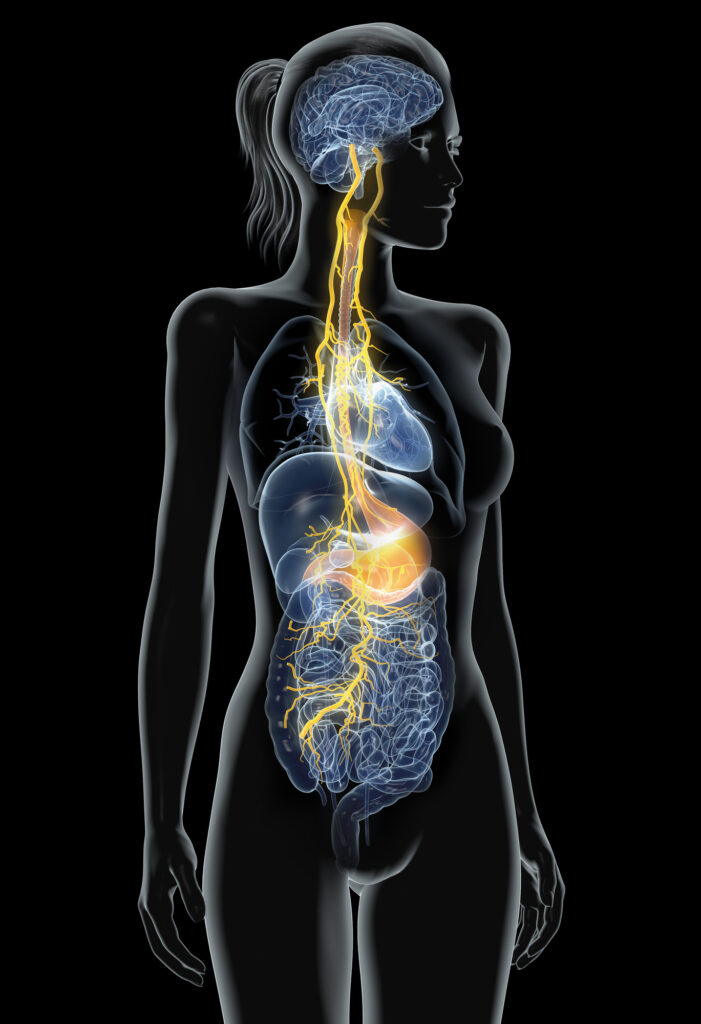
The gut and the brain are connected through a two-way communication system known as the gut-brain axis, which is heavily influenced by the gut microbiota. This axis has become a focal point of research in various fields that explore the underlying biological and physiological mechanisms of neurological, neurodevelopmental, psychiatric, and age-related disorders.
A close and remarkable connection exists between the gut and the brain. The brain and the gastrointestinal systems are derived from the same embryonic tissue. Both systems interact and communicate regularly, even sharing the same language in the form of neurotransmitters and peptide hormones. “Gut feelings” and butterflies in the stomach are manifestations of this connection.
Microbiota vs. microbiome, what the difference?
The human body is home to trillions of microorganisms, comprising bacteria, fungi, viruses, and other microbes that collectively form the microbiota. These microorganisms perform diverse functions, such as producing vital nutrients, regulating inflammation, and supporting immune system function. The microbiota also helps to maintain a healthy balance between harmful and beneficial bacteria in the gut, and when this balance is disrupted, it can lead to a range of health issues, including autoimmune diseases, mental health conditions, and digestive disorders.
The microbiome, which encompasses the genomic contribution of microorganisms, plays a critical role in various processes crucial for human survival, such as digestion, hormone synthesis, and immune system function. The type of microorganisms residing in the gut significantly influences human physiology, from cognitive function and immune system regulation to the body’s utilization and absorption of nutrients. In addition to providing essential nutrients and regulating bodily functions, these microorganisms produce neuroactive metabolites, including neurotransmitters and their precursors. As they digest our food, they send signals to the brain, which interprets and modifies the nervous system, inflammation, and other bodily processes accordingly.
Several factors can influence a person’s unique microbiota composition, such as the mode of birth delivery, childhood infections, use of antibiotics, nutrition and diet quality, environmental exposures, genetics, stress, and sleep. Therefore, maintaining a healthy microbiome is essential for human survival as it helps to promote a healthy and functioning body.
Signs of a Gut-Brain Imbalance
Dysregulation of the gut-brain axis has been linked to various disorders, including functional gastrointestinal disorders, mood disorders, and autoimmune disorders.1,2 Here are some common signs and symptoms of gut-brain axis dysfunction:
- Cognitive Functions: Negative impact on mental clarity, alertness, memory, stress response, mood, sleep, and focus.3
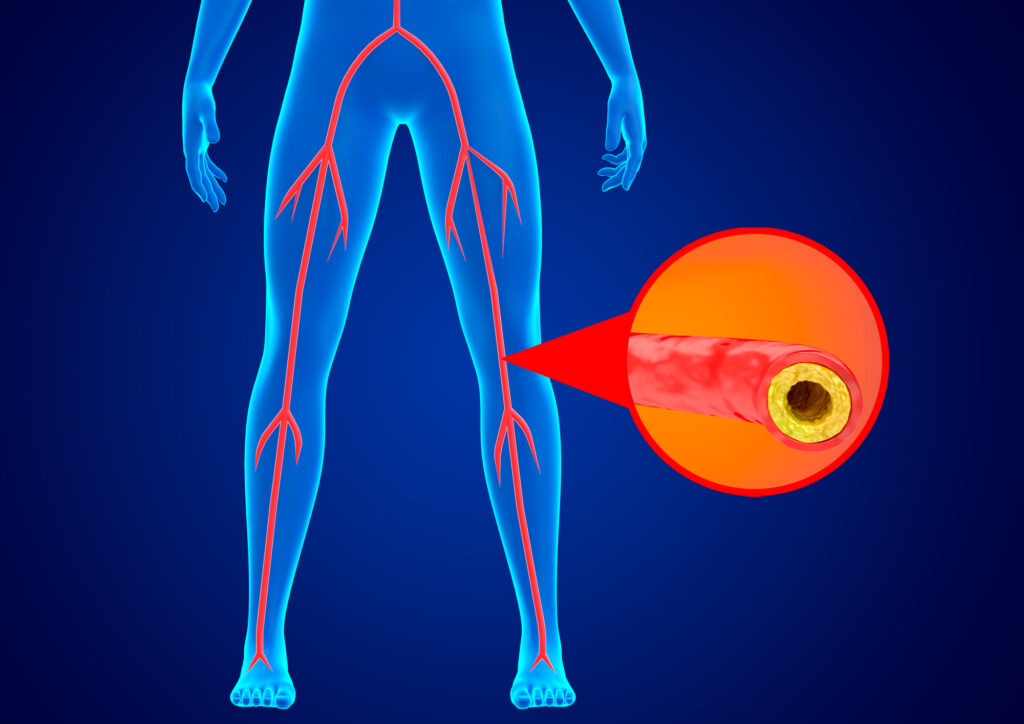
- Digestive problems: Dysregulation of the gut-brain axis has been associated with various gastrointestinal symptoms, including abdominal pain, bloating, diarrhea, constipation, IBS, and gastroesophageal reflux disease (GERD), all of which are associated with leaky gut.4,5
- Mood disorders: Studies have shown a correlation between gut-brain axis dysfunction and mood disorders such as anxiety, depression, mood swings, and irritability.6,7 New research has also shown a correlation with other major mood disorders such as schizophrenia.8
- Fatigue: Chronic fatigue syndrome (CFS) is a condition characterized by persistent fatigue that is not alleviated by rest and is often accompanied by cognitive impairment, headaches, and other symptoms. Studies suggest that gut-brain axis dysfunction may play a role in the development of CFS.9
- Autoimmune disorders: There is emerging evidence that dysregulation of the gut-brain axis may contribute to the development of autoimmune disorders such as rheumatoid arthritis and multiple sclerosis.10,11
- Skin conditions: Gut-brain axis dysfunction has been linked to the development of various skin disorders, including acne, rosacea, and atopic dermatitis.12
- Weight gain: There is evidence that alterations in gut microbiota and gut-brain signaling may contribute to the development of obesity and metabolic syndrome.13
- Food cravings: There is evidence that gut microbiota can influence food intake by regulating satiety signals and modulating reward pathways in the brain. Thus, dysregulation of gut-brain signaling may contribute to the development of food cravings and compulsive eating behaviors.14
How Does the Gut-Brain Axis Work?
Our brain and microbiome can exchange information in several ways. It involves sensory neurons in the gut that detect changes in the gut environment and send signals to the enteric nervous system. The enteric nervous system processes the sensory information and generates local reflexes that can modulate gut motility, secretion, and blood flow. The enteric nervous system also sends signals to the central nervous system via the vagus nerve. Hormones produced by gut cells can also enter the bloodstream and reach the brain, where they can modulate appetite, mood, and other physiological functions. The gut microbiota can also influence the gut-brain axis by producing neurotransmitters, short-chain fatty acids, and other metabolites, which influence many pathways, including:
- The immune system
- Tryptophan metabolism
- The vagus nerve
- The enteric nervous system
These pathways control the generation and assimilation of neuroactive chemicals, modulation of inflammation, and interaction with the vagus nerve by the gut microbiota. To learn more about the precise mechanisms of these pathways, and the role of specific microbes and neurotransmitters in gut-brain axis communication, continue reading: From Microbes to Mind: The Science of the Gut-Brain Connection Part 2.
Several reports indicate that the gut-brain axis can be influenced by supporting healthy intestinal barrier function, stress response and cellular function. Products that SFI Health offers that provide these primary support functions include Target gb-X™, Cortisol Management™, and Eicosamax® 1000.†
- Recognizing and treating disorders of gut-brain interaction. Harvard Health Publishing. Christopher D. Velez, MD. April 20, 2022 https://www.health.harvard.edu/blog/recognizing-and-treating-disorders-of-gut-brain-interaction-202204202730 Accessed March 1, 2023
- Carabotti M, Scirocco A, Maselli MA, Severi C. Ann Gastroenterol. 2015;28(2):203-209.
- Gomaa EZ. Human gut microbiota/microbiome in health and diseases: a review. Antonie Van Leeuwenhoek. 2020;113(12):2019-2040.
- Mayer EA. Nat Rev Neurosci. 2011;12(8):453-466.
- Mitrea L, Nemeş SA, Szabo K, Teleky BE, Vodnar DC. Front Med (Lausanne). 2022;9:813204.
- Foster JA, McVey Neufeld KA. Trends Neurosci. 2013;36(5):305-312.
- Chen Y, Xu J, Chen Y. Nutrients. 2021;13(6):2099.
- Bioque M, González-Rodríguez A, Garcia-Rizo C, et al. Prog Neuropsychopharmacol Biol Psychiatry. 2021;105:110130.
- Shukla SK, Cook D, Meyer J, et al. PLoS One. 2015;10(12):e0145453.
- Chu XJ, Cao NW, Zhou HY, et al. Rheumatology (Oxford). 2021;60(3):1054-1066.
- Kadowaki A, Quintana FJ. Trends Neurosci. 2020;43(8):622-634.
- Bowe WP, Logan AC. Gut Pathog. 2011;3(1):1.
- Torres-Fuentes C, Schellekens H, Dinan TG, Cryan JF. Lancet Gastroenterol Hepatol. 2017;2(10):747-756.
- Alonso-Alonso M, Woods SC, Pelchat M, et al. Physiol Behav. 2015;152(Pt B):479-486.