The commentary published on Today’s Practitioner from Jeffrey Bland PhD and Alex Vasquez, DO was met with widespread interest. In light of the response and the scientific flip flopping regarding Omega-3 fatty acids and coronary disease, it’s important to take retrospective look at a significant 2016 study, Polyunsaturated Fatty Acid Biomarkers and Coronary Heart Disease: Pooling Project of 19 Cohort Studies (JAMA Int. Med 2016) and a supporting editorial, published J Public Health Emergency 2017 by Philip Calder, BSc, PhD, DPhil, professor of immunology at University of Southampton. This article highlights Calder’s key points and offers the full text editorial to registered users at the end of this summary.
In his guest editorial, Professor Calder, BSc, PhD, DPhil, reviews the scientific history and outlines the overwhelming evidence showing that with conscientious consumption of marine sources of docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) and/or supplementation, the general public can indeed reduce their risk of coronary disease.
The following is a summary of Calder’s editorial with supporting references (if you prefer to read the full editorial, jump down to the full text button at the conclusion of this article).
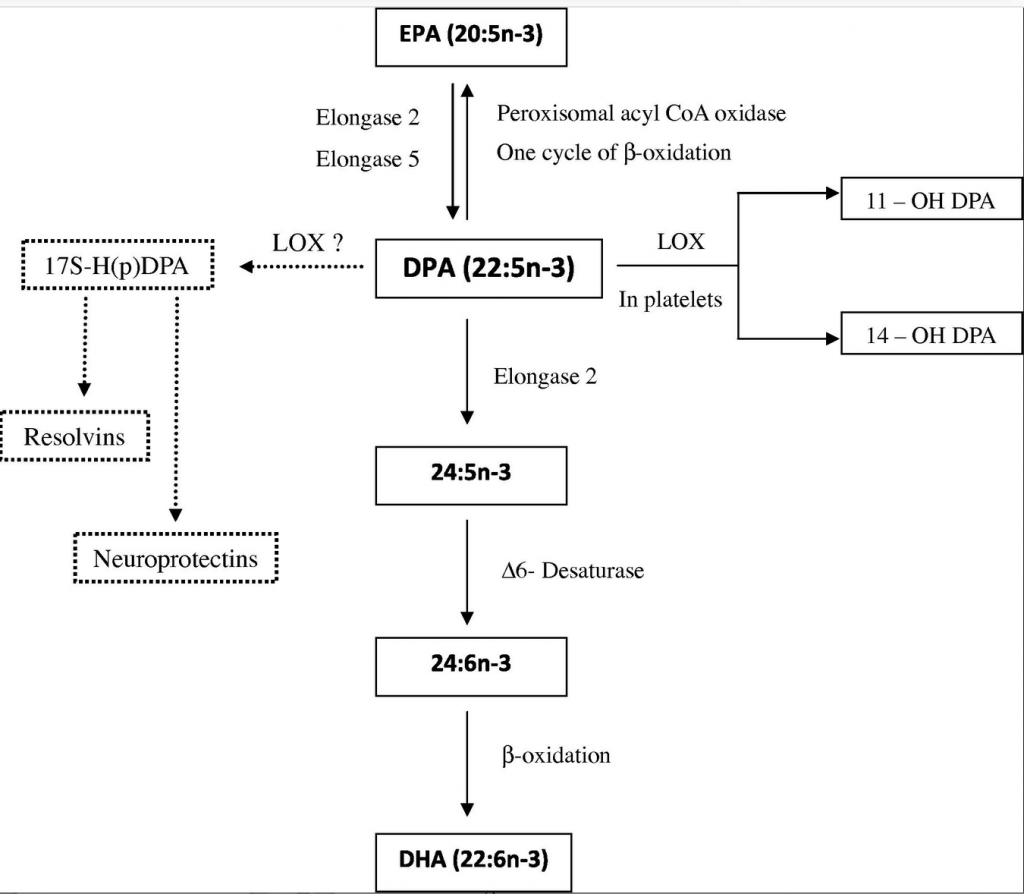
- Functionally the most important omega-3 fatty acids appear to be EPA (20:5n-3) and DHA (22:6n-3) (2,3), although roles for docosapentaenoic acid (DPA) (22:5n-3) are now also emerging.[1] There is growing evidence showing that DPA has beneficial effects in reducing inflammation and inhibiting aggregation in platelets and has a 10-fold greater endothelial cell migration ability than EPA, which is significant for wound healing. See FIGURE 1 and for more on DPA, see the full text link in the reference section below.
FIGURE 1
- A systematic review and meta-analysis collated prospective studies examining the association of dietary or circulating fatty acids, including omega-3 fatty acids, with risk of coronary outcomes.[2] Outcomes included fatal or nonfatal myocardial infarction, CHD, coronary insufficiency, coronary death, angina, or angiographic coronary stenosis. The aggregation of data from 16 studies involving over 422,000 individuals showed a RR of 0.87 [95% confidence interval (CI), 0.78–0.97] for those in the top third of dietary EPA plus DHA intake compared with those in the lower third of intake.
- In the same study cited above, there was no effect of dietary ALA intake using data from 7 studies involving over 155,000 individuals.2 The aggregation of data from 13 studies involving over 20,000 individuals showed RR of 0.78 (95% CI, 0.65–0.94), 0.79 (95% CI, 0.67–0.93) and 0.75 (95% CI, 0.62–0.89) for those in the top third of circulating EPA, DHA and EPA plus DHA, respectively, compared with those in the lower third.
- There has also been significant interest in the effect of omega-3 fatty acids in people with existing CVD, for example in survivors of myocardial infarction or in patients with heart failure. Several such studies published between 1989 and 2008 reported lower rates of death in patients receiving EPA and DHA at doses of 0.5 to 1.8 g/day for periods of 1 to 5 years.[3],[4],[5],[6]
- Meta-analyses of these studies were very supportive of a benefit of EPA and DHA in secondary prevention of mortality due to coronary causes [7],[8],[9] and pharmaceutical grade EPA and DHA began to be included in guidelines for secondary prevention of myocardial infarction in some countries. Calder makes two important distinctions: 1) It is likely that the mechanisms that reduce the likelihood of cardiovascular events and mortality in patients with established disease are different from the mechanisms that act to slow the development of atherosclerosis; i.e., different mechanisms operate in primary and secondary prevention. 2) Three key mechanisms have been suggested to contribute to the therapeutic effect of EPA and DHA. These are altered cardiac electrophysiology seen as lower heart rate, increased heart rate variability and fewer arrhythmias; an anti-thrombotic action resulting from the altered pattern of production of eicosanoid mediators that control platelet aggregation; and an anti-inflammatory effect which would act to stabilize atherosclerotic plaques preventing their rupture.
Calder further discusses the protective effects of DHA and EPA for patients within certain at-risk categories. Despite the positive findings with omega-3 fatty acid interventions in at-risk patient groups, which are supported by meta-analyses and biologically plausible candidate mechanisms, a number of studies published since 2010 have not replicated the earlier findings. This leads us to a where we are today: some studies show there is little protective effect of supplemental omega-3 fatty acids on cardiovascular mortality, especially in at-risk groups.
It is important to recognize that the most recent studies of omega-3 fatty acids and cardiovascular mortality in at-risk patients have been criticized for various reasons related to small sample size, the low dose of EPA plus DHA used, and the too short duration of follow up.[10] Nevertheless, these recent trials and meta-analyses have led to the conclusion that omega-3 fatty acids have no role in CHD or CVD prevention or treatment.”
Calder says this conclusion does not fit well with current evidence, which clearly demonstrates a role for EPA and DHA in primary prevention of CHD. He makes the case that the situation regarding secondary prevention remains unresolved as supportive meta-analyses continue to be published. Most of all, experiences with patient post-myocardial infarction is positive.[11]
Above all, Calder emphasizes that it is important to “separate the consideration of the effects of omega-3 fatty acids in primary and in secondary prevention since (I) different biological mechanisms are involved; and (II) primary prevention involves dietary habit over decades while secondary prevention typically involves shorter term use of omega-3 supplements.
In his conclusion, Calder writes: “The findings confirm a role for omega-3 fatty acids in primary prevention of coronary disease. An estimate of the intakes of EPA and DHA required to bring about an increase in EPA and DHA concentration that is protective suggests that such intakes are achievable in the general population.”
REFERENCES