As the initial impact of the COVID-19 pandemic subsides, health care practitioners are facing its weighty aftermath—long COVID, and its plethora of respiratory, neurologic, cardiovascular and other symptoms that can linger for weeks, months or even years following the initial infection. While researchers scramble for causes and cures, efforts are focusing on managing the condition and mitigating its devastating manifestations.
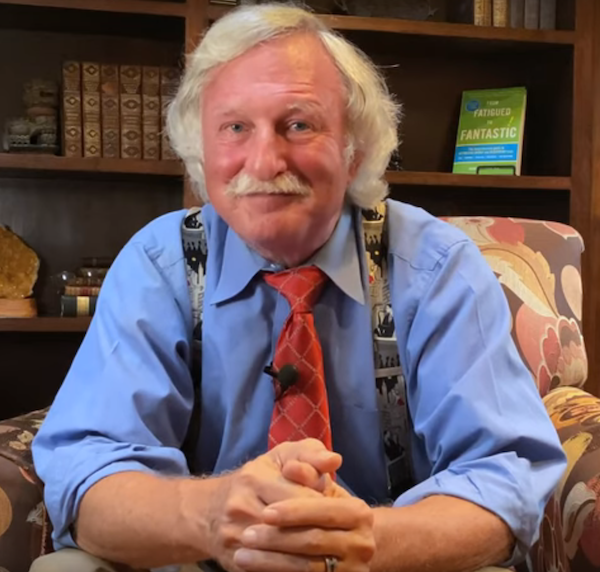
In this episode, we talk with Jacob Teitelbaum, MD about long covid and a treatment protocol he is using to improve the quality of life for patients dealing with the major disruptions due to long covid. Dr T is well known for his work helping patients with chronic fatigue syndrome.
“The fatigue, brain fog, pain and disordered sleep associated with long COVID simply reflect post-viral chronic fatigue syndrome and fibromyalgia,”says Teitelbaum. “These are very old conditions, and it took more than 40 years and hundreds of studies, including eight by me, to help us understand the causes and effective treatment of these conditions.”
Pharmacological approaches are limited: there are currently no medications for the condition itself, and drug therapies are purely symptomatic.
Originally designed to treat chronic fatigue syndrome and post-viral CFS, the SHINE
Protocol, developed by Dt T is an effective therapy for the unremitting fatigue and other complaints associated with long COVID. The SHINE protocol, which focuses on restoring energy production and reversing the effects of the hypothalamic and immune dysfunction.
Guest Bio:
Jacob Teitelbaum, MD, (a.k.a. “Dr. T”) is a board certified internist and nationally known expert in the fields of chronic fatigue syndrome, fibromyalgia, sleep and pain. He has authored numerous books including the best-selling From Fatigued to Fantastic! (now in its 4th edition). He is the lead author of numerous studies on effective treatment for fibromyalgia and chronic fatigue syndrome, and one study on effective treatment of autism using NAET. He also developed the popular free smartphone app “Cures A-Z.” Dr. T lives in Kona, Hawaii.
Contact: [email protected]
Links mentioned in the podcast:
Related Content:
Treating Long COVID: What We Know So Far Current findings shed light on its pathogenesis and progression—and offerpromising protocols to improve patient’s lives.
Covid-19 Resource Center – A collection of articles and research on the topic
Transcript:
Understanding Long Covid
/45:15/E1
Rob Lutz 00:03
Hello and welcome to the OneMedicine Podcast from Today’s Practitioner. In each episode, we share the expertise of a respected thought leader. Some you’ll know and others you’ll probably meet for the first time. We cover topics important to you, always with a focus on improving the health outcomes of the patients you treat, while expanding your understanding of the many healing modalities being used today. Welcome to the OneMedicine Podcast. I’m Rob Lutz. I’m the host and with me today is Dr. Jacob Teitelbaum, Dr. T. Quick bio on Dr. T – he’s a board certified internist and nationally known expert in the field of chronic fatigue syndrome, fibromyalgia, sleep, and pain. He’s authored numerous books, including the best-selling “From Fatigue to Fantastic.” He’s the lead author on numerous studies on effective treatment for fibromyalgia and chronic fatigue syndrome, and one study on effective treatment for autism using NAET. He also developed the popular free smartphone app called Cures A-Z. Dr. T lives in Kona, Hawaii. Welcome, Dr. T, to the OneMedicine Podcast.
Jacob Teitelbaum 01:07
Aloha and welcome everybody today, too. Thank you Rob, this is going to be a good time today for everybody. For those of you out there who are working with people with Long COVID, or even just any other cause of chronic fatigue and fibromyalgia, we’re going to organize all of this for you today, let you know what’s causing it, and how to make it go away all in a very “how-to” approach.
Rob Lutz 01:31
That’s great. So before we jump into the main topic of what we’re going to be discussing today, a couple of questions I’d like to ask you: I’m always curious how you went from a conventional training into a more of an integrative functional method…what happened? What was it that brought you…usually it’s some some event in your life that caused you to go down this path. Can you share with us a little bit about that?
Jacob Teitelbaum 01:54
Yeah, it’s like people ask: “What’s a nice doctor like you being a quack like this?” or something. The same way that most of us went through…I found myself on the other side of the white coat. Usually it’s us or a family member with it. It’s funny–I explain to people that being an MD is kind of like getting your bachelor’s degree, and then holistic medicine is when you continue and you get your master’s and your PhD. And people say, oh…okay. So basically my dad had died when I was younger. I was paying my own way through college. I finished college in two and a half years because you paid by the semester, so I just kind of rolled through it. I was in med school rolling through that, working as a nurse in Children’s Hospital, and that was all the easy part of my life. My family background is my mom was in Auschwitz; most of my family died in the camps and they all decided go through a meltdown and tried to put me in the middle. Emotionally…I was very smart, but emotionally, I had the depths of a teaspoon. Basically it was just that I couldn’t manage it. My uncle literally had a heart attack in my living room trying to manipulate me and to manipulate the other cousins. It was emotionally intense. So those are the setup for the drop in energy. And I got this nasty drop-dead flu, this nasty virus. It took me out of the game, triggered post-viral chronic fatigue syndrome and fibromyalgia. Since I was paying my own way, that left me homeless, sleeping in parks. I was in Tulsa on a park bench. It’s as if the universe put a holistic homeless medical school sign on the park bench. Naturopaths camp, I didn’t even know there was such a thing. I said: “You can actually practice doing that?” I was all set to go back and be a naturopath if I healed up, and the universe said no, you’re gonna be an MD. Long story…energy workers, chakra workers, herbalists…all these different people came by and they sat on my park bench and taught me. I was able to return to med school, got my honors in medicine, and have spent the last 47-48 years researching, teaching, writing books, doing studies on effective treatment for post-viral and other causes of chronic fatigue syndrome and fibromyalgia.
Rob Lutz 04:06
I guess it makes sense why you’re so focused on chronic fatigue, if that’s really what kind of brought you here in a lot of ways, right? Yeah. My other question and you kind of teed it up a little bit: So you had a lot of these different practitioners coming by, different focuses on what they called medicine. What do you call the type of medicine that you practice?
Jacob Teitelbaum 04:26
Comprehensive medicine? That’s a term coined by Dr. Hugh Riordan. Brilliant, underspoken gentleman who passed many years ago.
Rob Lutz 04:39
One final question: If there’s one unifying principle between all these different types of medicine that are out there, what what would you say that would be? What is the one thing that connects all these different types of medicine, whatever the modality might be or the name might be?
Jacob Teitelbaum 04:54
There’s no one thing; you have to look at the combination of the biophysics, the structural, the chemistry and the mind-body, or the biophysics and the mind-body. You have to do the whole thing. There’s no one-size-fits-all.
Rob Lutz 05:10
Got it. Perfect. Thank you. Okay, so now we’re going to jump into Long COVID. It’s it’s something that’s fairly prevalent; I think there was a recent study that just came out, they’re able to identify it based on some markers. But it sounds like it’s a very high percentage of people that have had COVID end up with Long COVID. So can you help me understand what is what exactly is Long COVID?
Jacob Teitelbaum 05:31
So it’s 10%. And again, that study was maybe the fifteenth test that’s positive. The powers that be prefer to make believe that this is all in people’s minds. When you do that, you don’t have to pay health benefits and disability benefits. But basically, we’re looking at 10% of people who get COVID get post-viral chronic fatigue syndrome. This translates to almost 20 million people in the United States. I would, simply put, view this as an energy crisis where people trip a circuit breaker. That’s the kind of organizing thing because you hear: Is it the toxins? Is it nutrition? It’s an energy crisis, okay, and then we can organize it from there. But one way to think of it starting, you can trip a circuit breaker in this disease in hundreds of ways, just like you can in your home, there’s no one way. But if you look at the post-viral: Viruses don’t have mitochondria, or at least not much in the way of energy producing organelles. They basically rely on hijacking the hosts, mitochondria and energy production. So our bodies, when it senses foreign DNA, viral DNA, shuts down energy production to try to starve the virus. And that works really well for a couple of days or a week. But sometimes, especially if there are little bits of viral particles leftover, the body won’t shut that process off, the low energy continues, and you’re stuck in this low-energy state. So you need to turn energy production back down for people to recover.
Rob Lutz 07:06
I see. So someone who has Long COVID as we described, are there those–I’m just curious–is there kind of a continuum or a spectrum that someone may not have the worst condition of Long COVID, but certain symptoms that may benefit from this protocol that you’ve been working on? Or those that have had COVID, maybe it’s not as bad as those that are technically with Long COVID? Do some of these treatment protocols work for those folks as well after they’ve had COVID?
Jacob Teitelbaum 07:33
Yes, and let me break it into two things. So what we’re going to talk about today works for fatigue and pain in general, often cognitive dysfunction. In terms of people with Long COVID, the current working definition for Long COVID–what’s the medical word–sucks. Horribly. You’ll see no useful research coming out. The NIH has really blown through the billion dollars with nothing therapeutically to show for it of benefit, where I could find two pet dogs and a rabbit that could have come up with at least treatments without money and research. It’s sad. They define long COVID as any persistent symptom after COVID. So for example, say we were trying to treat auto accidents and we lumped in skull fractures and sprained ankles, and all the other things in between, and you try to design a treatment. That’s silly. So I want to break that out. The most common things, if you look at symptoms post COVID, people will have lung damage, shock lung, ARDS. Again, use some Boswellia, use Curamed, which is a highly absorbed curcumin and clinical glutathione, shut down to free radical oxidative stress, shut down the inflammation. And the research shows it tends to heal on its own over about two years. People with heart disease, any heart disease, arrhythmias, angina, post-MI, heart failure, you want to increase cardiac muscle efficiency, it helps all of those. You look at the Cures A-Z phone app, nice simple recipe: Ribose, B vitamins, magnesium, acetyl carnitine, CoQ10. You will see in six weeks dramatic clinical improvement, whatever the cause of the heart injury, because the heart muscle efficiency improves and there’s more. But that’s a simple way to begin and you see very prominent effects. So those two things. I have free information sheets on a lot of the different topics so I’m going to fill those out. My email address is [email protected].
Rob Lutz 09:36
We’ll include that in the transcript as well. So when folks come back to the podcast, a lot of this information you’re sharing, I’ll make sure the links are there so they can find this information from you.
Jacob Teitelbaum 09:52
Perfect. So if people are coming in with shortness of breath, most of the time it’s not heart/lung. It’s vagal nerve. But you can email me for a shortness of breath after COVID information sheet that you can just modify for your practice and give out to people.
Rob Lutz 10:06
Okay, great. I’d like to talk about the vagal nerve at some point if we have time towards the end here, because I think that’s fascinating. I did work with…we’ve got an article on the on the website, Today’s Practitioner, where there’s a physical therapist who has come up with a protocol to work on the vagus nerve. And actually, he’s brought back taste and smell for patients who had lost that. So many things I find interesting with the vagus nerve, but that I found fascinating. So how exactly are we diagnosing Long COVID?
Jacob Teitelbaum 10:41
I tend to get excited about what I do, because it’s so treatable for people. The Long COVID we’re focusing on here is post-viral chronic fatigue syndrome, or fibromyalgia, often both together, most often. So how do you diagnose it? If you have somebody with fatigue and widespread pain, brain fog, or insomnia, any of those other three–fatigue and any of the other three–presume they have Long COVID. Started with COVID and persisted. It can start months after the COVID, too. I’m going to broaden that. If somebody comes in with severe unexplained fatigue and insomnia, that paradox–exhausted and can’t sleep, presume they took the hypothalamic circuit breaker, which is the sleep center, hormonal, autonomic control center. That circuit breaker. Can’t sleep, despite being exhausted. That’s enough for me to make that diagnosis, and to move forward with treating.
Rob Lutz 11:42
And what exactly do you do for that? Is it looking at cortisol levels and things like that? Or what exactly are you doing for a patient that comes in like that.
Jacob Teitelbaum 11:51
It takes a comprehensive approach, so we call it the SHINE protocol. So if you want to organize it–this worth writing down–point one, they’re exhausted and can’t sleep, they’ve tripped a circuit breaker that they’ve got to process. Point two, it’s an energy crisis. Point three, restore energy production and turn this circuit breaker back down with the SHINE protocol. That means you address sleep. And with Long COVID It’s only 40% who have the sleep issues initially, because in the first year you’re often oversleeping. And then it goes into insomnia once it gets past the first year, but you need to address sleep quality regardless.
Rob Lutz 12:34
So a question about that. I use a sleep app, you know, and I track how much REM and how much deep sleep. I may be asleep for eight and a half hours, but like last night, I think I had 30 minutes of REM and 10 minutes of deep sleep. So I didn’t feel very rested. is Is that what you’re looking at as well? I mean, of course, a lot of your patients may not have a sleep app of some sort or tracker, or are they just not sleeping? They just can’t fall asleep.
Jacob Teitelbaum 13:00
There’s all kinds of technology and I’m a very high-tech kind of guy. So, the technology I recommend is asking people, how long does it take to fall asleep? How often do you wake up during the night? What’s your total night’s sleep? And do you feel rested in the morning? That’s gonna tell me what I need to know. You’ll find me very high-tech all the way through the show today. Simple questions will do that. So if they’re waking and they’re feeling like they have non-restorative sleep, they have trouble falling asleep, trouble staying asleep, they have sleep-disordered breathing like sleep apnea, or UARS. All of these will tell you with those four questions? How do I address it? Number one, we all know the sleep hygiene kind of stuff: Don’t load up on coffee right before bedtime. Don’t sit there trying to watch what we call–it’s the thing on TV where they try to scare everybody if it doesn’t make them hate each other. It’s a fiction–oh, the “evening news.” Turn all that off; I don’t care what side you’re watching. It’s a fiction meant to scare you to death and to make you hate everybody because that’s good for business. And that will get you watching, but it’s not good to watch that before bedtime because how the hell are you going to fall asleep right after watching that kind of stuff? People need a sleep routine. There are sleep herbals; there’s a wonderful mix called the revitalizing sleep formula. I designed that; well, my royalties go to charity blah, blah, blah…mix the six herbs. There’s the terrific ZZZZ, there’s EP120. Euromedica makes some wonderful products; they make an EP120 sustained release 10 milligram melatonin. I take that myself because you want a sustained release that will keep you out through the night. So you can start with these simple things. When using medications, because they may be needed, the Z medications tend to help initiate sleep, but to maintain sleep, tiny doses of trazadone, 25 milligrams–flexural, two and a half milligrams–gabapentin, 100 to 300. There’s a list of other natural and prescription things. But it’s like, if you’re go into a Chinese apothecary, the old Chinese guy opens up 50 drawers, takes a pinch of each, puts it all together. It’s more like that than a whole glob of one. Low doses of several things get people sleeping through the night without being hung over. the next day.
Rob Lutz 15:19
So sleep, is that kind of the cornerstone to this, would you say? It really is and probably for so many things. Sleep is critical.
Jacob Teitelbaum 15:29
You can’t get rid of pain and you can’t get your energy back if you’re not sleeping.
Rob Lutz 15:33
Makes sense. So let’s keep going through the SHINE protocol; what would be next?
Jacob Teitelbaum 15:38
H stands for hormones and hypotension, basically POTS kind of things. So the hormones are low across the board; the hypothalamic pituitary axis controls almost every hormone in the body. At least the endocrine hormones. And the tests, it’s important. I love asking the question when I’m speaking with physicians, which is where does the normal range lab tests come from? Now, the holistic doctor guys really know this, but when I ask it to standard practitioners, like 400 doctors is kind of like looking at 400 deer in the headlights. “I have no idea.” We were given the impression that the world’s experts, wise old men with silver beards that all look like Gandalf are sitting around the table and they say, “Well, if it’s in this normal range, no problem!” There’s no such thing. The normal range is simply two standard deviations; you take 100 healthy people, you do the test, the highest and lowest 2% are abnormal, and the 95% in the middle are the normal rrange. I explain it to patients in a way that’s easy to understand: The normal range for shoe sizes is size 6 to 13. And normal income is $8100 a year in two standard deviations. $16,000 is the poverty. But the doctor will say, “If you’re $8100 a year income and a size 6 shoe, no problem at all! As long I’m not the one having to wear it.” So the tests give you an idea where people are in the overall population. The symptoms tell you: Do they need a thyroid–tired, achy, weight gain, cold intolerant–two of those, I’m going to give them a trial of the desiccated thyroid. We could spend three hours talking about whether you’re synthroid, desiccated, T3–the bottom line is everybody’s different. And reverse T3, if that’s high, that may push me more to the T3. But I’m usually going to start with desiccated thyroid. If they get too jittery, I’ll go to synthroid. If they just don’t get a response, but they still sound hypothyroid, I’m going to go to the T3 protocols, but those again, making them hyperthyroid biochemically, with high doses of T3. But you want to adjust it to what feels best for the person while keeping the free T4 from being elevated. Low is okay; you put people on T3, the T4 and TSH will go way down. That’s fine.
Rob Lutz 18:24
So, you’re you’re asking the patient questions and you’re taking that information and deciding what to give them. Are you then also testing to see where these levels are going after they’re starting to take this? Or are you still just going back to the questions?
Jacob Teitelbaum 18:38
I’m testing, but I’m relying predominantly on symptoms. So if their free T4 is in the top 10% or higher, I’m going to lower the dose unless they really, really need the higher dose clinically. That’s when you start seeing the toxicity. A low TSH–TSH is a piece of crap test, Rob, I’m sorry. Especially if you have hypothalamic dysfunction and you’re relying on a TSH, that’s insane. You may as well just be broadcasting an old “I Love Lucy” rerun on your windshield and try to drive based on that. It’s a meaningless test. I adjust it to what feels best to the person while making sure the free T4 is not elevated for safety.
Rob Lutz 19:22
So what other hormones are you looking at?
Jacob Teitelbaum 19:24
Adrenal. Another study just came out that found that low cortisol, not low based on the adrenal insufficiency going to kill you, but significantly lower than the healthy population. And we’ve, of course, all of this we’ve been saying for 30 years and we’ve known that and they’re coming up with: “Oh, look what we found!” Well, you know, the Earth has been here a while; this is all old stuff. So how do I diagnose low adrenal in this disease? Again, I’ll do the testing. If the morning fasting cortisol is under 14, I suspect–again, do the salivary indexes if you’d like–but if I had to keep all the tests or one question, I would keep one question: Do you get irritable when hungry? Do you get hangry? And if their spouse is with them and going “yes”…if people get irritable when hungry, they have low adrenal and that should be addressed. Naturally, I have a product called Adrenaplex that has a mix of glandulars, licorice, pantothenic acid, C, tyrosine, DHEA, pregnenolone, it’s all in one or two capsules a day. It’s really sweet, easy, Adrenalplex. One or two a day will smooth most problems.
Rob Lutz 20:43
Is that a branded formula or does that come from one particular company?
Jacob Teitelbaum 20:48
That also is Euromedica. Sometimes I will use hydrocortisone in more severe cases. And I’m very comfortable using it up to 20 milligrams a day, which is like four milligrams of prednisone. One of my earlier studies showed you do not get adrenal insufficiency at 20 milligrams or less a day. It begins at 25. You don’t suppress the adrenal. There’s no suppression of 20 or less. And the toxicities have been shown with prednisone, except for adrenal suppression, which starts at 5 milligrams, most of the toxicity besides acid stomach and some fluid retention begins at 7 milligrams. But I’m very comfortable when needed going somewhere between two and a half to 20 milligrams of hydrocortisone a day, and if people need it for the rest of their life, that’s okay.
Rob Lutz 21:40
At that dosage? You think it’s okay?
Jacob Teitelbaum 21:42
I think it’s safe at that dosage. The first time I heard that I said, “What crazy person is this?” I spent three years not just looking at Professor Jeffries’ work, but going through the literature saying, “There must be studies.” And all there were were people saying, “Well, this other person says that any dose is toxic,” and they refer back, and that person eventually refers to the first person. Nothing. I couldn’t find anything. The osteo, the cataracts, and maybe loss of bone density. There aren’t studies for the lower dose, but most of the other toxicities are dose-related. Your body makes the equivalent of 35 milligrams of cortisone a day. So if you’re giving 20 and your body doesn’t want it, it will make less. When you go higher, the body no longer has control, so the adrenal, certainly DHEA and pregnenolone, I will check and supplement those as needed as well.
Rob Lutz 22:36
Any other hormones that you’re paying attention to?
Jacob Teitelbaum 22:38
Reproductive. Again, all the hormones are on this circuit. So reproductive hormones, and again, the blood tests for women, for estrogen, progesterone, and FSH, LH will not go deficient, go down until the person has been deficient for 5 to 12 years. That is a very late finding. How do I diagnose? Again, simple question, are your fibromyalgia symptoms worse around your menses? Not your PMS. Not this little progesterone, but if you’re having headaches, fatigue, brain fog, insomnia, achiness–all of these are worse around your menses, it’s low estrogen and progesterone.
Rob Lutz 23:24
What about post-menopause?
Jacob Teitelbaum 23:28
If they’re past the menses, and they have a fibro, I’ll finesse this just to do that. But the vaginal dryness suggests it and if the FSH and LH are over 80s, I’m pretty quick to give a trial of the vaginal bioidentical hormone replacement, including one to five milligrams, usually one to two milligrams, of testosterone. There’s work out of Dartmouth University showing that even with normal testosterone levels, women given low dose of testosterone in fibromyalgia–it’s Professor Hillary White–had decreased fibromyalgia pain.
Rob Lutz 24:08
Interesting. Why do you think that is?
Jacob Teitelbaum 24:10
Well, fibromyalgia is critical for tissue repair. It’s also critical to increase your blood cell mass. And this disease, what you’re finding is people have decreased blood volume, and the low–so the hermatocrit is okay because volume is low, they’re dehydrated, and your blood cell count is low. But since they’re both low, they cancel out on the tests and it looks normal. But if you do a nuclear scan for red blood cells and blood volumes, that’s all in the tank. Why? Because the next hormone, anti-diuretic hormone and the fluid- and salt-controlling hormones and the hypothalamus. Basically, people are leaking like buckets that are full of holes. They can’t hold onto water or salt. They need a lot of salt water. Even if they’re drinking the four times that everybody else is, they’re peeing five times as much.
Rob Lutz 25:02
Wow. So what do you do to treat that? You’re looking at all these different hormones and based on the symptoms that you’re getting from the patient, and you’re coming up with a very specific treatment protocol for each patient, or there’s some similarities between all of these, would you say?
Jacob Teitelbaum 25:17
It’s tailored to each person. There’s a simple–I actually hold a US patent for a computerized physician…it’s expired already, but I created that a long time ago, because people with fibromyalgia couldn’t get help otherwise–it’s called energyanalysisprogram.com. It’s free. People can go in, put in their symptoms, put in their pertinent lab tests, it will analyze all of them and determine which of these 100 variables are most active in their case. I can’t say it’s a fibromyalgia program because then I’d have to pay $100 million to the FDA. That’s an energy analysis program to fix the energy deficits. So you’ll see it’s really good for people; they can go out and get the results. And it’s a simplified–I used to have it that it made the whole medical record for the person before they ever walked into the office. So most people in the thyroid, if they get hangry, give them Adrenaplex and salt and water, load them. That’s the simple. And then, men and women bioidentical hormone replacement. Testosterone is under 500 in men? Or are they showing symptoms of metabolic syndrome? Erectile dysfunction? The symptoms of low testosterone? I’m going to treat–the 208 normal range is absurd.
Rob Lutz 26:33
Are you seeing some of your patients with Long COVID with these types of symptoms as well?
Jacob Teitelbaum 26:39
Yeah, and the reproductive hormone deficiencies develop more over time. The adrenal is almost immediate; the thyroid kind of in between. So I go on to symptoms. And again, it’s like, “What if I’m wrong, and they don’t have it?” Then they won’t feel worse on it. Stop it.
Rob Lutz 26:56
Right.
Jacob Teitelbaum 26:59
You’re trying on shoes. Simple as that.
Rob Lutz 27:00
Instant feedback, right? Any other hormones?
Jacob Teitelbaum 27:04
Those are the main ones. But what I would do, we talked about the low adrenal and the low blood volume, which leads to the other part of H, which is hypotension. It’s a misnomer. But if it’s a sign, stick it in there. This is basically orthostatic intolerance, Postural Orthostatic Tachycardia Syndrome, that’s an alphabet soup. POTS is the one in vogue now. When we stand up, we’re a big bag of water. Think of what gravity does with all our blood; it sends it down to our legs. We had to develop autonomic function to send blood back up to the brain and heart and muscles and the rest. Otherwise, again, we may be dizzy, over time brain foggy, achy, and tired. So you don’t need tilt-table testing. You don’t. That’s a horrible, expensive, nasty test that’s not reliable. If you email me at [email protected], ask for the Long COVID information, I’ll automatically send that, because the majority of people have it. It’s a simple test you can do. You have them lie down for 10 minutes, and they can do this at home, check their pulse, and then have them stand in one place and check their pulse every minute or two for 10 minutes. If at any time during that, it goes up over 20 beats a minute, if they have the fatigue and the symptoms, it’s suspicious. If it goes over 30 beats a minute higher, it confirms it. It’s easy.
Rob Lutz 28:34
Just to touch on that for a second. So, you have them lay down for 10 minutes, so their heart rates come down. They’re kind of at a resting heart rate. Then they stand up and they’re just going to stand there for 10 minutes, and they’re going to take their pulse. And if it goes up 20 to 30, then for you that’s a major symptom to look at.
Jacob Teitelbaum 28:50
They’ve got it. They’ve got POTS or whatever letters you want to put on it; it needs to be treated. And again, increased salt, increased water, adjust the adrenal compression stockings. Now again, most people don’t want to wear old lady stockings, the medium pressure thigh high. But you know, if you have somebody’s who’s bedridden, they’re kind of game with it. But even the athletic ones, the ones the athletes wear that say “added compression.” They look sharp, and people will wear them. The higher the better, but even knee-highs add something. And then there’s half a dozen medications and there’s other supplements. The vagal, the autonomic training, if we have time at the end, we’ll talk about ANS Rewire or Dynamic Neural Retraining System. Those help as well. So very, very, very treatable, once you know it’s there.
Rob Lutz 29:42
Very good. So that’s the H. Anything else on the H that we should cover? Okay, so the next is I.
Jacob Teitelbaum 29:48
I will be infections. So again, the immune system goes initially on overdrive, because it’s ramped up, and then it exhausts itself. So you’ll see the natural caloric activity goes down, you’ll see different phases. I wouldn’t spend a nickel for those tests because we know their immune system is fighting and then exhausted and overwhelmed. And you’re going to get opportunistic infections, which means infections that a healthy immune system keeps at bay. We know Epstein-Barr reactivates and Long COVID, that’s been shown again. We know in CFS and fibromyalgia, there’s multiple viral reactivation. So people say, “Oh, well, yeah, everybody’s test is positive for Epstein Barr antibody.” Yes, even healthy people walking the street, 95% of adults are positive. It doesn’t mean squat. Now there are ranges you can have where you see if they’re in the top 10%. But these tests being positive means nothing. And the few very rare ones that I’ve seen the Epstein-Barr IgM be positive, don’t seem to be helped by treatment. We can do the testing if it will make you feel better. But the bottom line if they have recurrent viral kind of flu-like symptom feelings, you can do things like ThyroPro and a good multivitamin. I go with a Famvir/Celebrex protocol. Again, my book “From Fatigue to Fantastic,” that blue guy over my shoulder, it’s all laid out. You can ask me for it, I can cut and paste it for you.
Rob Lutz 31:24
Again, we’ll include your email address and links to your site in different places, so they get this information.
Jacob Teitelbaum 31:30
It takes 4 to 6 months. You’ll start with adding the Celebrex, which is strangely antiviral. It blew my mind, but it is. Those two are synergistic by themselves, neither of them too much.
Rob Lutz 31:43
Why are these infections staying in the body? Is it like in a biofilm? What’s happening? Where are they still there?
Jacob Teitelbaum 31:51
The immune system is exhausted because it got cranked up and never turned off. Can you imagine if you had an army that their horns are blowing and then somebody put the record player for the “charge” thing on and a month later nobody turned it off, and the soldiers are still running all over the place? They’re exhausted. That’s what’s happening to your immune systems and this disease. The most important infection or one of the most important is candida overgrowth. This is a massive organism. If a virus is–in relative terms–the size of a period at the end of a sentence, and spirochetes might be as big as a room, and Candida as big as a city block. I mean, these parasites are in the same scale. These are massive for our immune system to fight. You’re playing fantasy board games, and this is like the biggest giant on the field coming by. So there’s no test I would give a nickel for Candida. Plenty of tests, but they don’t correlate with whether people get better taking the treatments. I don’t think they’re useful. How do I diagnose Candida in this disease? Chronic nasal congestion that’s not allergic, it’s not seasonal. Chronic sinusitis, irritable bowel syndrome, gas, bloating, diarrhea, constipation, any of those. And Fibromyalgia. I will treat with diflucan, 200 milligrams a day for six weeks. Or there’s a whole host of natural antifungals; we all have our favorites. But they need extended periods, the good probiotic. But the six weeks of diflucan is very helpful. ITC compounding pharmacy, it’s a mail order, will make the sinusitis nose spray, which combined with the diflucan is brilliant. It’s by prescription. Again the Candida, for me…so if I had to pick one treat. Most people have and get…most people get…they will flare and it hurts when you first treat it, so start slow and work up. But it makes a massive difference in outcome for people. Most of you out there know about Lyme disease. So all I need to say about post-Lyme is that persistent symptoms after the antibiotic means it may have tripped the circuit breaker. You need to go ahead with the SHINE protocol and low dose Naltrexone that we’ll talk about as time allows. Then your antibiotics, they’re gonna have persistent benefits from the antibiotic treatments that you’re doing for the Lyme and co-infections. But that’s a whole other three-hour discussion. People already have their own protocols.
Rob Lutz 34:30
Living here in the Northeast, Lyme is a is a big issue. It seems to be getting bigger, too. So maybe we can have another episode and talk about Lyme.
Jacob Teitelbaum 34:39
I would have Neil Nathan on for that one. I’m in microtoxins. So he’ll be good. But my book will go through it in depth and many other books on that as well. So you have all these infections that when the immune system is down they come in, but the book will talk about also when to use antibiotics. The Lyme tests are not reliable. And they’ll go through: Do they have scalp sores? Zithromax helps their whole body with that for some reason. Wait, that’s a marker. Chronic lung congestion? Have they taken an antibiotic? “Hey, I took amoxicillin for dental work; my CFS went away.” “No, what happened when they kept you on it?” “Oh, they wouldn’t give it to me.” “What?” “They said, ‘Well, I can’t give me long-term antibiotics.'” I said, “Did you say you have acne?” “Hey, I went back and said I had zits; they gave me two years of tetracycline, no problem.” So, treat the infections.
Rob Lutz 35:28
Treat the infections. Anything else you want to talk about with regard to the infections, I? No. Okay.
Jacob Teitelbaum 35:34
We have about five to eight minutes; let me wrap up with two key areas. One is nutritional support. A good multivitamin high in B vitamins, magnesium, I use the essentials multivitamin, a coenzyme Q10. But they have one now with gamma cyclodextrin. Euromedica makes this one, too. It’s a chewable. They have a bunch of them; get the chewable 100 milligram. It’s equivalent of 700 milligrams of CoQ10. There are two studies we recently completed; one was a form of red ginseng. It’s called red ginseng energy with HRG80 red ginseng. It increased energy in this population about 60% n average. Stamina went up, sleep improved, cognition improved, it was–in fact, if you look at the one thing I have on my desk, it’s a bottle of the ginseng energy. That’s remarkable.
Rob Lutz 36:28
Is that a separate product from the chewable with the CoQ10?
Jacob Teitelbaum 36:32
The chewable CoQ10 is a separate product and the red ginseng energy, but you want the chewable, too. Keep your eyes out for gamma cyclodextrin added to products. It’s a natural compound that increases absorption seven-fold, so people aren’t taking handfuls of pills all day. You’ll find what I’ve tried to do here is give you the smallest number of capsules and pills. So people can do it.
Rob Lutz 36:56
To make it easier, because too many pills, they’re just not going to be compliant with a protocol, right? What other nutritional support do you recommend?
Jacob Teitelbaum 37:05
I’m going to repeat: Increase salt, increase water, avoid sugar. Otherwise, see what diet leaves you feeling the best overall. For most people, it’s a high protein diet with frequent grazing or snacking through the day. But for some people, they go keto type diet, they get depressed, they need the carbs. So see what feels best to the individual. Some people thrive with a vegetarian diet and others look like they’re Kwashiorkor kids. So it really needs to be tailored to the individual.
Rob Lutz 37:35
Any thoughts around intermittent fasting for something like this?
Jacob Teitelbaum 37:38
It can help. Again, you have the insulin resistance tends to be a part of it. Food sensitivities are often a part of it. In terms of symptomatic relief, the keto diet is more likely to help than intermittent fasting. For weight loss, intermittent fasting is great,
Rob Lutz 37:55
Okay, so that’s nutritional support. Anything else?
Jacob Teitelbaum 37:58
Exercise. Don’t push excess exercise. Exercises able, light walking, if they have orthostatic intolerance, if you can get them exercising horizontally, rowing machine, or horizontal bike, because otherwise they stand up and exercise. Blood rushes to their legs. So once you’ve got them conditioned a little bit, lightly, lightly, a little bit of weight exercise. If you overpush, they will be bedridden for three days. If you try to be coaching them–More! More! Give me two more!–you’ll kill them. Not quite. But let’s not…don’t do that. Let them slowly, slowly condition. Now, why do they have pain? Pain and fibromyalgia predominantly begins because the low energy has caused some muscles to get locked in a shortened position. Think about it. If you have a heavy workout and your muscles get drained of energy, you don’t come home and say, “Honey, my muscles, they’re all loose and limp.” You go, “They’re all tight; they’re like a spring.” It takes more energy to stretch them. Low energy gets locked in a shortened position; your muscles are all tight. “Honey, can you rub my shoulders?” When you have low energy in the body, the muscles get locked in a shortened position. They’re tight and they hurt and the pain will move all over the place as you shift weight to try to unload the muscles. Once you have chronic pain in the muscles, it will trigger–any chronic pain–will trigger microglial activation, central sensitization, blah, blah, blah…brain, pain…which then triggers small fiber neuropathy or nerve pain. So 45%, 44% will have paresthesias. Everybody’s different but that’s most common progression. Treat pain; treat with SHINE. The studies show that most people no longer have fibromyalgia by the end of three months; the pain goes away. And it’s something called curafen which is a mix of an herb which is a pain relief miracle for people. Give that six to eight weeks. And then the book goes through each kind of pain. My Cures A-Z app, we’ll do that for free. There’s a two-buck upgrade, but most of the info is in the free app. Almost all pain is treatable. So those of you out there treating people with CRPS, email me for the CRPS information sheets, but just email me for the articles. Now I’m treating Long COVID, treating Fibromyalgia I’ll include the orthostatic intolerance along with the SHINE protocol. I’ll send the low-dose naltrexone; we don’t have time for that today, but low-dose naltrexone is two thumbs-up on this disease. Start slow, because you’re gonna mess with their sleep. But firstly, all pain can be eliminated. You just need to treat…it’s like the oil light in your car. You can try to put a bandaid on it or smash it or cut it out. What’s this medical approach? That doesn’t work very well. You put oil in the car, the oil light goes out. You give your body what it needs, the pain goes away.
Rob Lutz 40:49
Well, I know lack of sleep, people that don’t sleep at all, they seem to have a lot of pain just in general.
Jacob Teitelbaum 40:55
That’s what the research shows. You sleep-deprive people, they develop widespread muscle pain, which then will progress. Sleep is when you make growth hormone. That’s what helps with the tissue repair. That’s when the night crew is out repairing micro-damage to the tissues we have in the muscles all day.
Rob Lutz 41:13
Yeah, very connected, right? So how did you come up with this SHINE protocol? We’ve got a few more minutes. I’m just curious. Where did it come from?
Jacob Teitelbaum 41:23
I was on the road and I learned there was an adrenal issue. So I took adrenal support. I realized that since I was paying my own way through college and med school, I had the diet from hell. I was definitely sugarholic…
Rob Lutz 41:40
Snicker bars and Top Ramen and Dr. Pepper.
Jacob Teitelbaum 41:45
Those are the good days. So I had the Candida and the nutritional issues. I started with those and the energy work. And that was enough to get me back into med school. But over time, I realized okay, well I gotta get the sleep going. And I learned these things piece by piece. Professor Jeffries taught me about the adrenal things in more depth. Billy Crook about the candida issues in more depth. Janet Travell, these are the three doctors. Dr. Riordan, who my books are dedicated to. Each of them taught me bits and pieces, and it’s kind of like, “Oh, this is the answer!” And I would dive in. And I’d realize, “Oh, it was a little piece.” I would distill that piece down. And then there was another one. “Oh, this is…and this is…and this is.” And about 40 things later, I was like, “Okay, how do we organize this for people?” And I was on the Dr. Oz Show, and Dr. Oz is a good man; the Monsanto and pharmaceutical industry got pissed off at him. And they put their hired hounds into media and Congress. Notice how they all suddenly jumped on him; I can tell you stories firsthand of their just making crap up that I know firsthand. But when I was on his show, he said, “Well, okay, Jacob, this is interesting. I’m gonna send you somebody; get them well.” It was this lieutenant in the Air Force, and she came, and six weeks later, she was well. He said, “Now you can come on the show.” I called it the SHIN protocol in the earlier editions. I gotta add an E to make it SHINE. Okay, so that’s how SHINE came.
Rob Lutz 43:09
I like it. That’s great. So one last question: Is there any kind of a clinical pearl or bit of wisdom that you’d want to share? Something you’ve learned along the way that you just feel would be a great thing to share with the audience.
Jacob Teitelbaum 43:21
If you get people better so they go back to what made them sick in the first place, number one, we’ve done nothing for them, and two, something else will come along. They will be hit by a truck; I guarantee you it will always be the other driver’s fault. And they come right back out of the game again. So, for any severe chronic illness, once you’ve treated the physical components and they are able to hear it, and they’re getting better, guide them. Use your energy, use your improved health, to do what feels best to you, to be authentic, not to go spitting nickels so some other rich people are taking care of bureaucratic paperwork. The illness taught you that you don’t have to do those thirteen bags of paperwork; you didn’t get arrested, you’re not homeless. If that’s the case, let those go. And do the things…follow your bliss. That will be–it’s like, I tease that people should get a superpower like Spider-Man got bit by a spider and he got Spidey powers. The superpower from this disease, as we recover, is authenticity. It’s learning to say no to things that feel bad and learning to be authentic and do those things that make you feel good that make your heart sing without hurting anybody else.
Rob Lutz 44:30
That’s great. That’s a great message. And I do love that quote from Joseph Campbell: “Follow your bliss.” I did that a long time ago myself. Thank you so much for joining us. We’ll see you again soon.
Jacob Teitelbaum 44:43
A pleasure and an honor. Aloha, everybody.
Rob Lutz 44:45
Thank you so much. Thanks for listening to the OneMedicine Podcast. I hope you found today’s episode interesting and came away with a few insights you can apply to your practice. If you’re looking for the show notes, they can be found in the link below. If you want to go deeper on this topic, or anything else, please visit todayspractitioner.com and consider registering for our weekly newsletter as well. Thanks again, and I hope you’ll join us next time.

LISTEN ANYWHERE