In this study, researchers explore the advantages of an active complementary and integrative therapy for long-term, chronic-pain management. Active-pain management employs self-hypnosis, relaxation techniques and mindfulness practices in a home setting, but only if the patient is adequately educated beforehand.
This study shows that the ideal pain management model of care transitions the patient through some forms of passive care, such as acupuncture and massage during acute pain with transition care to chiropractic and/or osteopathic manipulation, and eventually leading to an active form of care for long-term solutions. Published in Global Advances in Health and Medicine, by David Cosio, PhD, Erica Lin PharmD, April 2018. Full text available at the end of this post.
In this study, held in Veterans Affairs medical setting, participants attended a Pain Education School and were educated about active treatment options and self-administered pain protocols outside the clinical setting. The study included 243 veterans (103 completed the study) and excluded anyone with cancer pain. Overall, the study found that those who were educated in active treatment options felt empowered to manage their pain without medication, surgery or ongoing practitioner provided treatments. Conversely, long-term, passive-pain management resulted in a feeling of disempowerment, and largely placed the onus back on the healthcare provider to relieve the pain.
The primary purpose of the current study was to investigate whether completion of a formal patient pain education program would increase utilization of active versus transitional and active versus passive CIH among Veterans.
Active-Pain Management Study Parameters
Potential candidates had several characteristics, including having failed medical/surgical treatment, exhibited an over reliance on medications/therapies, displayed pronounced inactivity, suffered from significant depression or anxiety related to his/her pain, demonstrated inadequate coping skills, and/or appeared receptive to adopting a self-management approach to pain management.
Each Veteran was subsequently scheduled for 11 weeks of 1-hour classes. Participation in subsequent classes was voluntary. Veterans were encouraged to bring significant others when they attended classes. The Veteran sample had mixed idiopathic chronic, non-cancer pain conditions, including back pain (75%), neck pain (13%), extremity pain (7%), head pain (3%), and fibromyalgia/soft tissue pain (2%). Most Veterans were African American (58%), but 36% were Caucasian, 5% identified as being Hispanic/Latino, and in 1% race was unknown. Most were males (82%) and 18% were female Veterans.
As part of the introduction and at the last session of the program, all Veterans completed a pre- and post-education assessment. The assessment included questions which asked Veterans if they had ever been treated by specific Complementary and Integrative Healthcare (CIH) modalities. This questionnaire was adapted from the Complementary and Alternative Medicine (CAM) Questionnaire ß, SECTION A: Use of Alternative Health Care Providers. The choices included the following active, transitional, or passive modalities:
- Active: acceptance and commitment therapy/mindfulness, biofeedback/relaxation training, hypnosis, movement programs, music/art therapy, and spirituality/religion.
- Transitional: chiropractic care and osteopathic manipulation.
- Passive: acupuncture, aromatherapy, healing touch, massage therapy, and traditional healers.
Nearly 44% (N = 45) of Veterans reported not using any type of CIH at the baseline. The 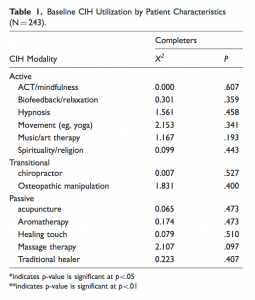
Lecturers just introduced the CIH modalities and did not provide any inducement for use. Veterans could ask questions and receive authoritative and useful answers from the providers themselves at the end of each class. Veterans also had access to each CIH modality immediately after it was presented in the program—patients did not have to wait till the completion of the program to begin seeking treatment.
Approximately 16% of Veterans reported not using any type of CIH after completing the Pain Education School program; which is more than a 25% difference from the baseline. The remaining 84% of Veterans reported increases in different combinations of CIH after completing the patient education program, including active (24%), passive (12%), and transitional (14%) CIH modalities. The researchers noted:
People who suffer from chronic pain tend to go for short-term relief at a long-term cost. Perhaps the reason why patients gravitate to passive treatments is because medical providers have reinforced the belief that these treatments are the standard of care for chronic pain management which has led to their participation. Scholars in pain medicine have recommended that providers focus more on offering active treatments and utilize passive interventions as an adjunct to chronic pain management. Active techniques have a synergistic rather than a mere additive effect when combined with other interventions. Active treatments have the added benefit of reinforcing the self-management approach to pain management, as opposed to passive interventions which have been shown to put the responsibility back in the providers’ hands.”
Conclusion / The results of the current study substantiate past research findings which indicate increased use of CIH modalities when additional education is provided about their availability. The current study further confirmed that there was a shift away from passive to more transitional and active CIH modalities upon completion of the pain education program. Thus, the program was found to be more aligned with the goal of pain management—that patients engage in more self-management.
Source: David Cosio, PhD,ABPP and Erica Lin, PharmD,BCAC. Role of Active Versus Passive Complementary and Integrative Health Approaches in Pain Management, Global Advances in Health and Medicine. April 10, 2018. doi.org/10.1177/2164956118768492
CLICK HERE TO DOWNLOAD THE FULL TEXT STUDY





