The emerging emphasis on oxidative stress, and science-based supplements shown to support conception.
Infertility is a widely recognized and rapidly increasing problem, affecting about 15 percent of couples worldwide. In the United States, fertility has largely followed a downward trajectory, falling to a record low in 2020 when 43 states recorded their lowest fertility rates in three decades. And while interventions have historically focused on women, male infertility is a common issue, involved in 30 to 50 percent of cases. The etiology of male infertility is not completely understood: environmental, behavioral and genetic factors are implicated, but in one in three patients, a specific cause is still not identified. Now, a growing body of evidence highlights the role of oxidative stress in disorders of sperm production, maturation or function and seminal fluid quality. What the research shows, and promising new approaches for treating male infertility.1, 2
Male infertility: influences and interventions.
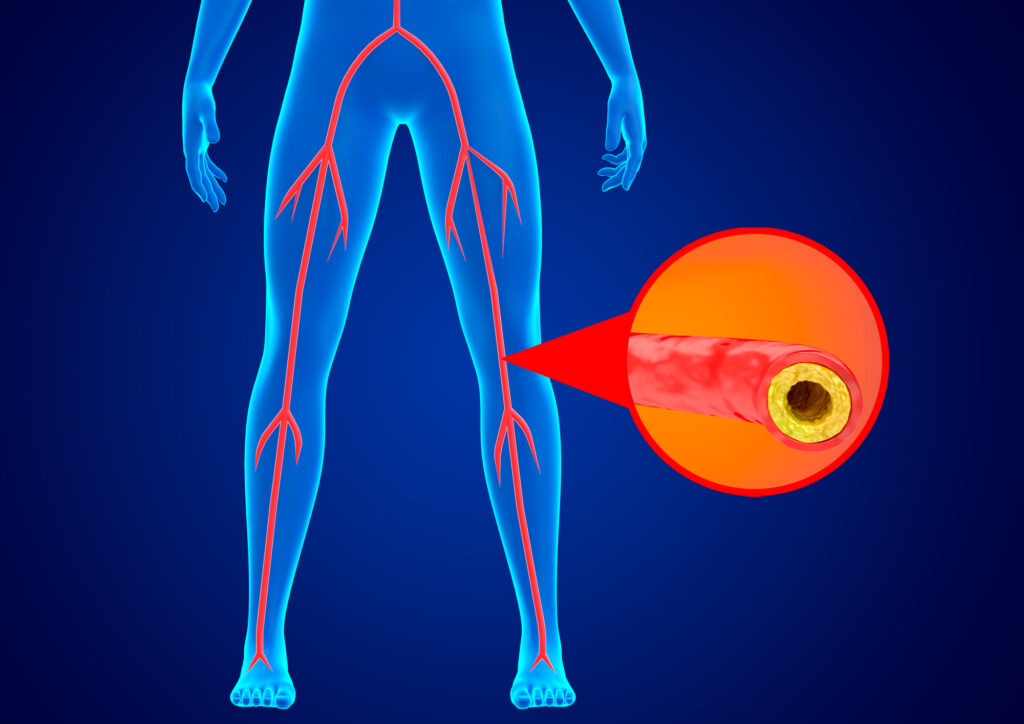
The causes of male infertility are broad and varied, each with different influences on diverse aspects of spermatogenesis. Genetic factors, hormonal imbalances or disorders, testicular damage, infection or injury, and medical conditions like varicocele are all known to affect sperm parameters. Lifestyle, behavioral and environmental factors are significant: excessive alcohol consumption, smoking, certain medications, including testosterone replacement therapy, and exposure to chemicals, pesticides or heavy metals diminish sperm quality and male fertility.3, 4, 5, 6
Obesity, chronic stress and insufficient sleep are linked with decreased sperm production and motility. A sedentary lifestyle negatively affects sperm parameters, but excessive exercise, especially cycling and other intense activities that raise scrotal temperature, have been shown to impair sperm production and function. Diets rich in fruits, vegetables and lean protein promote sperm quality, while increased intake of sugar and trans fats are linked with lower sperm counts, reduced motility and abnormal morphology.7, 8, 9, 10, 11, 12
Along with dietary interventions aimed at correcting deficiencies, specific nutrients can support sperm quality and enhance fertility, primarily by protecting against reactive oxygen species (ROS) that impact spermatogenesis and decrease male fertility. Emerging research emphasizes the strong association between oxidative stress and poor semen quality. Studies suggest 30 to 80 percent of infertile men have elevated seminal levels of ROS, and antioxidant therapy is considered a cornerstone of male infertility treatment.13, 14, 15
In addition to addressing diet, lifestyle and environmental influences, a personalized protocol should include evidence-based antioxidants proven to protect against ROS, promote healthy sperm parameters and foster fertility.
Science-backed supplements for supporting male fertility.
Zinc’s antioxidant properties shield sperm from ROS production and DNA damage, and adequate intakes improve sperm morphology, viability and motility. Deficiencies are correlated with a decrease in male fertility: zinc levels in the seminal plasma of infertile males have been shown to be lower compared to controls, and one meta-analysis found zinc concentrations in seminal plasma were positively associated with male fertility. In other studies, supplementation significantly increased sperm volume, sperm motility and percentage of normal sperm morphology.16, 17, 18
Folate is important for DNA synthesis and integrity, and low levels are related to a higher risk of sperm chromosomal abnormalities. Folic acid is known to counteract ROS and decrease inflammation, and studies link deficiencies with impaired spermatogenesis and reduced sperm concentration. While findings are mixed, evidence suggests folic acid supplementation can enhance male fertility, and in one review, folic acid alone showed the potential to improve sperm motility and IVF–ICSI outcomes.19, 20, 21
Vitamin D has both antioxidant and anti-inflammatory properties, and research points to its protective effects on DNA and cell membranes. Vitamin D levels are correlated with sperm parameters, especially motility, and several trials demonstrate a link between deficiencies and reduced sperm motility, sperm count and semen quality. Other interventional studies found vitamin D supplementation significantly increased sperm motility and rate of pregnancy.22, 23, 24
Omega-3 fats, primarily DHA, are essential for sperm cell flexibility and movement, vital to sperm performance. Imbalanced ratios of omega-6 to omega-3 can impair sperm quality and motility, and research suggests men with fertility issues had higher omega-6 to omega-3 blood ratios compared to fertile men. DHA has known antioxidant and anti-inflammatory properties, and in one meta-analysis, omega-3 supplementation boosted DHA concentrations and positively influenced sperm motility in men with fertility problems.25, 26, 27
L-carnitine, found in high concentrations in the male reproductive tract, plays a crucial role in energy metabolism and spermatozoa maturation. The antioxidant properties of L-carnitine protect against ROS, and studies show L-carnitine maintains sperm function, enhancing motility and epididymal function. L-carnitines supplementation is linked with significant improvements in sperm parameters and positive impacts on male fertility. Other research suggests L-carnitine supplementation reduces ROS levels, promotes sperm quality and increases fertility rates, even at a relatively low dose of 2 grams per day.28, 29, 30
Coenzyme Q10 (CoQ10) is involved in mitochondrial energy production, essential for maintaining the efficient energy system of spermatozoa and protecting their membranes from lipid peroxidation. Diminished levels are associated with several conditions determining infertility, such as varicocele and low sperm concentrations, and a number of studies link higher blood and seminal plasma CoQ10 with increased sperm count, motility and morphology. Supplementation has been shown to improve sperm parameters, including significant increases in total sperm counts and sperm cell motility, and some research suggests CoQ10 boosts fertility and total pregnancy rates.32, 33
About CoQ10: why ubiquinol is better.
While CoQ10 is effective, ubiquinol—a reduced and more absorbable form of CoQ10—is a superior approach to enhancing sperm quality and promoting male fertility. When CoQ10 is taken as a supplement, it must be converted to ubiquinol. The efficiency of conversion is affected by various factors, including genetic influences, nutrient deficiencies and certain medications, and ability to convert CoQ10 to ubiquinol markedly declines with age. Taking ubiquinol directly as a supplement bypasses the conversion process, providing the body with the active form of CoQ10. It’s also highly bioavailable, with studies showing ubiquinol is two to four times better absorbed than conventional CoQ10.34, 35, 36
In terms of its impact on male fertility, research points to a strong correlation between sperm count, motility and ubiquinol concentration in seminal fluid. Ubiquinol has been shown to improve multiple sperm parameters, with significant increases in sperm count, density, motility and morphology seen after daily ubiquinol supplementation of 150 to 200 mg.37, 38, 39
Other research demonstrates its efficacy in supporting male fertility:
- An open-label, six-month study of men with low sperm count found that supplementing with 150 mg of ubiquinol once daily lead to a 53 percent increase in sperm count, a 26 percent increase in total sperm motility and a 41 percent increase in absolute numbers of rapidly swimming sperm, compared to placebo.41
- In a retrospective six-month study of men with low sperm motility and abnormal sperm morphology but normal sperm count, fast-moving sperm increased from 5.7 percent to 11.5 percent, and sperm morphology improved from 2.6 percent to 3.1 percent, with 100 mg of ubiquinol twice a day, compared to placebo.42
References:
- Pew Foundation. Survey: The Long-Term Decline in Fertility—and What It Means for State Budgets. 5 December 2022.
- Isidori AM et al. Medical treatment to improve sperm quality. Reprod Biomed Online. 2006;12:704–714.
- Finelli R et al. Impact of Alcohol Consumption on Male Fertility Potential: A Narrative Review. Int J Environ Res Public Health. 2021 Dec 29;19(1):328.
- Bundhun PK et al. Tobacco smoking and semen quality in infertile males: a systematic review and meta-analysis. BMC Public Health. 2019 Jan 8;19(1):36.
- Patel AS et al. Testosterone Is a Contraceptive and Should Not Be Used in Men Who Desire Fertility. World J Mens Health. 2019 Jan;37(1):45-54.
- Kumar N, Singh AK. Impact of environmental factors on human semen quality and male fertility: a narrative review. Environ Sci Eur. 2022; 34, 6.
- Whirledge S, Cidlowski JA. Glucocorticoids, stress, and fertility. Minerva Endocrinol. 2010 Jun;35(2):109-25.
- Liu MM et al. Sleep Deprivation and Late Bedtime Impair Sperm Health Through Increasing Antisperm Antibody Production: A Prospective Study of 981 Healthy Men. Med Sci Monit. 2017 Apr 16;23:1842-1848.
- Kilic M et al. The effect of exhaustion exercise on thyroid hormones and testosterone levels of elite athletes receiving oral zinc. Neuro Endocrinol Lett. 2006 Feb-Apr;27(1-2):247-52.
- Durairajanayagam D. Lifestyle causes of male infertility. Arab J Urol. 2018 Feb 13;16(1):10-20.
- Salas-Huetos A et al. Dietary patterns, foods and nutrients in male fertility parameters and fecundability: a systematic review of observational studies. Hum Reprod Update. 2017 Jul 1;23(4):371-389.
- Çekici H, Akdevelioğlu Y. The association between trans fatty acids, infertility and fetal life: a review. Hum Fertil (Camb). 2019 Sep;22(3):154-163.
- Hussain T et al. Unraveling the harmful effect of oxidative stress on male fertility: A mechanistic insight. Front Endocrinol (Lausanne). 2023 Feb 13;14:1070692.
- Ahmadi S et al. Antioxidant supplements and semen parameters: An evidence based review. Int J Reprod Biomed. 2016 Dec;14(12):729-736.
- Agarwal A et al. Male Oxidative Stress Infertility (MOSI): Proposed Terminology and Clinical Practice Guidelines for Management of Idiopathic Male Infertility. World J Mens Health. 2019;37:296–312.
- Mousavi Esfiokhi SH et al. Effect of different sources of dietary zinc on sperm quality and oxidative parameters. Front Vet Sci. 2023 Jun 20;10:1134244.
- Allouche-Fitoussi D, Breitbart H. The Role of Zinc in Male Fertility. Int J Mol Sci. 2020 Oct 21;21(20):7796.
- Zhao J et al. Zinc levels in seminal plasma and their correlation with male infertility: A systematic review and meta-analysis. Sci Rep. 2016 Mar 2;6:22386.
- Yuan HF et al. Effect of folate deficiency on promoter methylation and gene expression of Esr1, Cav1, and Elavl1, and its influence on spermatogenesis. Oncotarget. 2017 Apr 11;8(15):24130-24141.
- Karahan G et al. Paternal MTHFR deficiency leads to hypomethylation of young retrotransposons and reproductive decline across two successive generations. Development. 2021;
- Li X et al. Effects of folic acid and folic acid plus zinc supplements on the sperm characteristics and pregnancy outcomes of infertile men: A systematic review and meta-analysis. Heliyon. 2023 Jul 13;9(7):e18224.
- Maghsoumi-Norouzabad L et al. Evaluation of the effect of vitamin D supplementation on spermatogram, seminal and serum levels of oxidative stress indices in asthenospermia infertile men: a study protocol for a triple-blind, randomized controlled trial. Nutr J. 2021 Jun 2;20(1):49.
- Adamczewska D et al. The Association between Vitamin D and the Components of Male Fertility: A Systematic Review. Biomedicines. 2022 Dec 29;11(1):90.
- Cito G et al. Vitamin D and Male Fertility: An Updated Review. World J Mens Health. 2020 Apr;38(2):164-177.
- Hishikawa D et al. Metabolism and functions of docosahexaenoic acid-containing membrane glycerophospholipids. FEBS Lett. 2017 Sep;591(18):2730-2744.
- Safarinejad MR et al. Relationship of omega-3 and omega-6 fatty acids with semen characteristics, and anti-oxidant status of seminal plasma: a comparison between fertile and infertile men. Clin Nutr. 2010 Feb;29(1):100-5.
- Hosseini B et al. The Effect of Omega-3 Fatty Acids, EPA, and/or DHA on Male Infertility: A Systematic Review and Meta-analysis. J Diet Suppl. 2019;16(2):245-256.
- Aliabadi E et al. Effects of L-carnitine and L-acetyl-carnitine on testicular sperm motility and chromatin quality. Iran J Reprod Med. 2012 Mar;10(2):77-82.
- Khaw SC et al. l-carnitine and l-acetylcarnitine supplementation for idiopathic male infertility. Reprod Fertil. 2020 Dec 23;1(1):67-81.
- Mateus FG et al. L-Carnitine and Male Fertility: Is Supplementation Beneficial? J Clin Med. 2023 Sep 6;12(18):5796.
- Safarinejad MR. Efficacy of Coenzyme Q10 on Semen Parameters, Sperm Function and Reproductive Hormones in Infertile Men. J Urol. 2009;182:237–248.
- Balercia G et al. Coenzyme Q10 supplementation in infertile men with idiopathic asthenozoospermia: An open, uncontrolled pilot study. Steril. 2004;81:93–98.
- Salvio G et al. Coenzyme Q10 and Male Infertility: A Systematic Review. Antioxidants (Basel). 2021 May 30;10(6):874.
- Miles MV et al. Bioequivalence of coenzyme Q10 from over-the-counter supplements. Nutr Res. 2002;22:919-929.
- Langsjoen PH, Langsjoen AM. Comparison study of plasma coenzyme Q10 levels in healthy subjects supplemented with ubiquinol versus ubiquinone. Clin Pharmacol Drug Dev. 2014;3(1):13-17.
- Evans M et al. A randomized, double-blind trial on the bioavailability of two CoQ10 formulations. J Funct Foods. 2009;1:65-73.
- Gvozdjáková A et al. Coenzyme Q₁₀, α-tocopherol, and oxidative stress could be important metabolic biomarkers of male infertility. Dis Markers. 2015;2015:827941.
- Alleva R et al. The protective role of ubiquinol-10 against formation of lipid hydroperoxides in human seminal fluid. Mol Aspects Medicine. 1997;18 Suppl:S221-S228.
- Balercia G et al. Coenzyme Q10 levels in idiopathic and varicocele-associated asthenozoospermia. Andrologia. 2002;34(2):107-111.
- Safarinejad MR et al. Effects of the reduced form of coenzyme Q10 (ubiquinol) on semen parameters in men with idiopathic infertility: a double-blind, placebo controlled, randomized study. J Urol. 2012 Aug;188(2):526-531.
- Thakur AS et al. Effect of Ubiquinol therapy on sperm parameters and serum testosterone levels in Oligoasthenozoospermic infertile men. J Clin Diagn Res. 2015;9(9):BC01-BC03.
- Cakiroglu B et al. Ubiquinol effect on sperm parameters in subfertile men who have astheno-teratozoospermia with normal sperm concentration. Nephro Urol Mon. 2014;6(3):e16870.