Scientists have developed two complementary bladder models to study urinary tract infection (UTIs) caused by E. coli: bladder organoids and a bladder-on-a- chip. The two studies reveal how bacteria invade the bladder, and how they evade the immune system and resist antibiotics. The studies, published in the journals Cell Reports and eLife, provide researchers and clinicians with a powerful new for studying the pathogenesis and treatment of UTIs.
Urinary tract infections (UTIs) are among the most common bacterial infections. They usually require treatment with antibiotics, and almost a quarter of treated cases lead to recurrent infection. The vast majority of UTIs are caused by a subspecies of the bacterium Escherichia coli, which infect cells that line the bladder wall and form what are known as “intracellular bacterial communities.”
The “communities” repeatedly rupture and bacteria re-enter neighboring cells, eventually killing off the so-called “umbrella cells” that line the outermost layer of the bladder’s epithelium. The loss of umbrella cells then allows the bacteria to invade the deeper layers of the bladder, where they can form “quiescent intracellular reservoirs” that are resistant to antibiotics and cause UTI recurrences. The dynamics of these events are hard to capture in vivo in animal models.
“Infection dynamics are difficult to capture from static imaging of tissue explants at serial time points,” says Kunal Sharma, the lead author on the two studies. “Thus far, in vitro models have not recapitulated bladder architecture with sufficient fidelity to study the time course of these events.”
Bladder Organoids and Bladder-in-a-Chip
To address this, the group of Professor John McKinney at EPFL’s School of Life Sciences developed two complementary bladder models to study UTIs in a more controlled way. The first model consists of bladder organoids that recreate the 3D stratified architecture of the bladder epithelium. Organoids are tiny lab-grown tissues and organs that are anatomically correct and physiologically functional.
The second model is a bladder-on-a-chip that incorporates physiological stimuli, e.g. the mechanical effect of bladder filling and voiding, as well as an interface with the vasculature to study immune cell migration to sites of infection.
“By generating organoids from a mouse with a fluorescent label incorporated within cell membranes, we could use live-cell confocal imaging at EPFL’s BioImaging & Optics Core Facility to identify specific bacterial niches within the organoid with a high spatial resolution,” says Sharma. “By imaging multiple organoids, we managed to identify heterogeneity and diverse outcomes of host-pathogen interactions. This proof-of-concept system has shown promising potential for follow up studies on bacterial persistence to antibiotics and the dynamics of immune cell responses to infection.”
In combination with volumetric electron microscopy performed by EPFL’s Biological Electron Microscopy Facility, the researchers found that solitary bacteria rapidly invade into deeper layers of the bladder, independently of the formation of intracellular bacterial communities, where they are protected from antibiotics and host immune cells. These findings could be leveraged to improve UTI treatment strategies.
In the complementary bladder-on-chip model, the researchers looked at the growth dynamics of bacteria within intracellular bacterial communities over time. They grew human umbrella and endothelial cells together under a simulated urine-flow system, and applied mechanical stresses to mimic the natural expansion and contraction of the bladder.
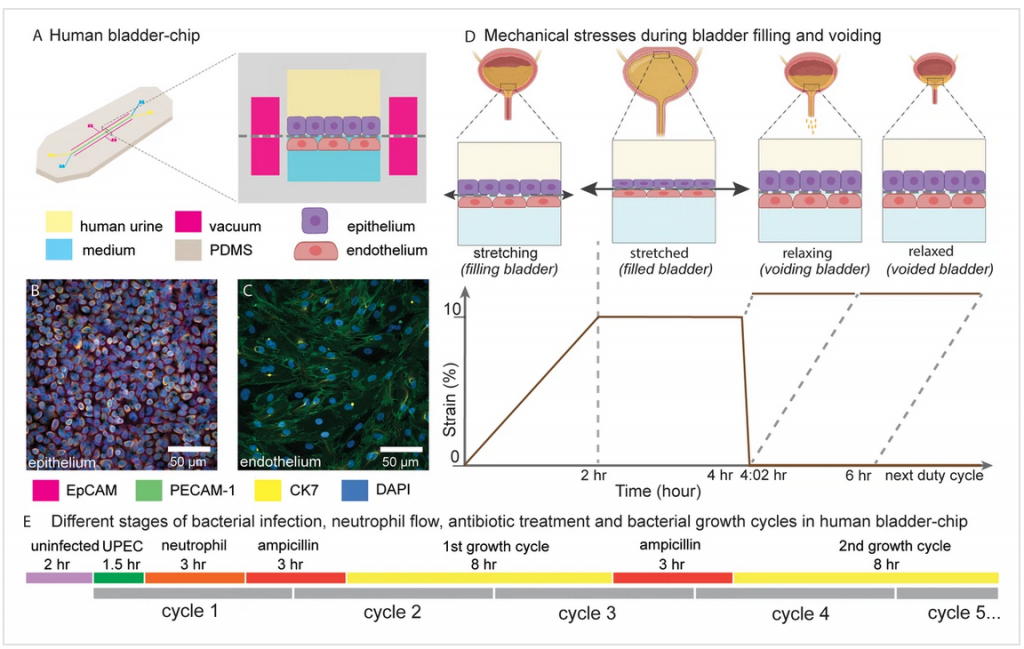
This study focused on the role of neutrophil recruitment in response to infection, revealing that neutrophils cannot eliminate intracellular bacterial communities. By tracking intracellular bacterial communities over successive cycles of antibiotic treatment, the researchers found them to be highly dynamic and resistant to antibiotics.
“These studies are part of the NCCR-funded “AntiResist” consortium aimed at developing more realistic in vitro models for infectious diseases, and using this knowledge to develop optimal treatment strategies, which could potentially have an enormous impact on human health,” says McKinney.
“Microphysiological models bridge the gap between simple cell culture systems and animal models,” says Vivek V. Thacker, a senior author on both studies. “The two models complement each other well and are tailored to study specific aspects of the disease. We hope they will serve as a resource for the wider microbiology community and advance the synergies between the tissue engineering and infectious diseases communities.”
Conclusion/ “The researchers found that by using time-lapse microscopy, the rapid recruitment of neutrophils from the vascular channel to sites of infection leads to swarm and neutrophil extracellular trap formation but does not prevent IBC formation. Subsequently, we tracked bacterial growth dynamics in individual IBCs through two cycles of antibiotic administration interspersed with recovery periods which revealed that the elimination of bacteria within IBCs by the antibiotic was delayed, and in some instances, did not occur at all.”





