One of the most commonly used diagnostic tools, particularly during this pandemic, is the reverse transcriptase polymerase chain reaction test (RT-PCR) for COVID-19 tests. By using a person’s respiratory sample, laboratory professionals across the U.S. and the globe have used RT-PCR to find out if a person has been infected with SARS-CoV-2, the virus that causes COVID-19.

These tests have played a critical role in our nation’s response to the pandemic. But, while they are important, researchers at Johns Hopkins have found that the chance of a false negative result — when a virus is not detected in a person who actually is, or recently has been, infected — is greater than 1 in 5 and, at times, far higher. The researchers caution that the predictive value of these tests may not always yield accurate results, and timing of the test seems to matter greatly in the accuracy.
“It is critical to understand how the predictive value of the test varies with time from exposure and symptom onset to avoid being falsely reassured by negative test results.”
In the report on the findings published May 13 in the journal Annals of Internal Medicine, the researchers found that the probability of a false negative result decreases from 100% on Day 1 of being infected to 67% on Day 4. The false negative rate decreased to 20% on Day 8 (three days after a person begins experiencing symptoms).
They also found that on the day a person started experiencing actual symptoms of illness, the average false negative rate was 38%. In addition, the false negative rate began to increase again from 21% on Day 9 to 66% on Day 21.
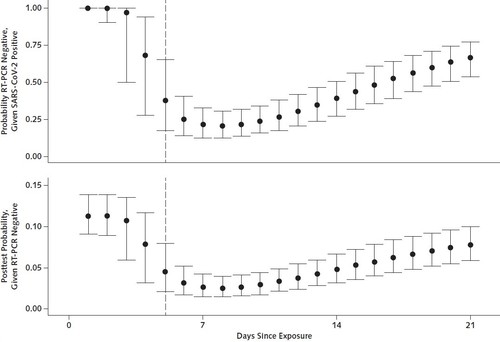
The study, which analyzed seven previously published studies on RT-PCR performance, adds to evidence that caution should be used in the interpretation of negative test results, particularly for individuals likely to have been exposed or who have symptoms consistent with COVID-19.
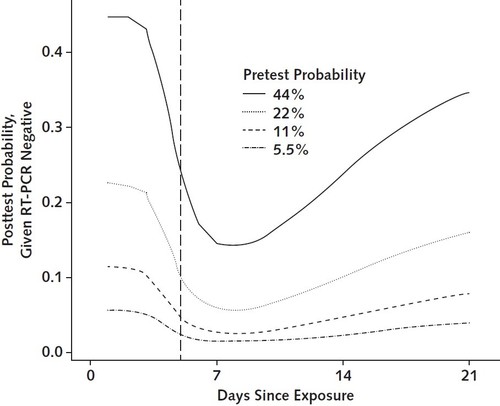
Conclusion/ “In summary, care must be taken when interpreting RT-PCR tests for SARS-CoV-2 infection, particularly early in the course of infection and especially when using these results as a basis for removing precautions intended to prevent onward transmission. If clinical suspicion is high, infection should not be ruled out on the basis of RT-PCR alone, and the clinical and epidemiologic situation should be carefully considered. In many cases, time of exposure is unknown and testing is done on the basis of time of symptom onset. The false-negative rate is lowest 3 days after onset of symptoms, or approximately 8 days after exposure. Clinicians should consider waiting 1 to 3 days after symptom onset to minimize the probability of a false-negative result. Further studies to characterize test performance and research into higher-sensitivity approaches are critical.”