One particular probiotic strain found in supplements — Bacillus subtilis — was shown to dramatically reduce Staphylococcus aureus (S. aureus) in the gut without killing off friendly bacteria, according to a study in Lancet Microbe.
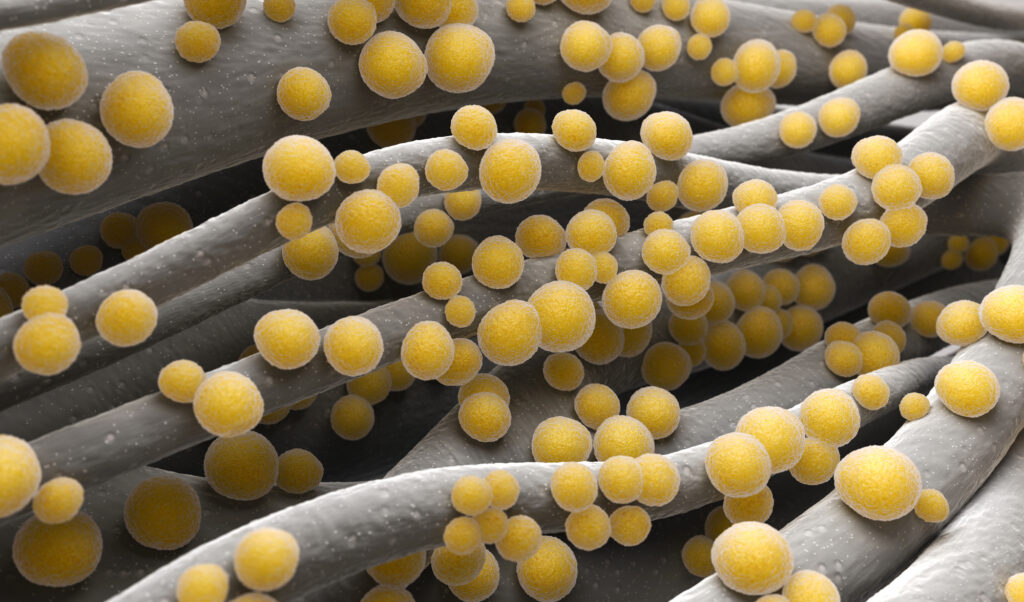
S. aureus is a bacterium commonly associated with skin infections. But if it enters the bloodstream, the microbe can cause dangerous antibiotic-resistant infections. This includes strains of methicillin-resistant S. aureus (MRSA), often called superbugs.
Naturally present on the skin and in noses, S. aureus also lurks in the gut where it is nearly impossible to eradicate with antibiotics, as antibiotics kill both bad and beneficial bacteria.
In a 2018 human study, researchers discovered that people with Bacillus in their stool had no S. aureus in their bodies. For reasons yet unknown, about one-third of people have a colony of S. aureus in their bodies. Other findings suggest that Bacillus subtilis (B. subtilis) offers protection against S. aureus.
For the current study, scientists wanted to know if Bacillus subtilis could target and destroy S. aureus without harming the gut’s healthy microflora population.
Study Details
The research team worked with 115 healthy adults from Thailand, all of whom had nasal and stool samples positive for S. aureus. The subjects were randomly divided into two groups, taking either a B. subtilis supplement daily or a placebo for 30 days.
The results were impressive: B. subtilis killed off a whopping 97% of S. aureus in the gut, on average. And levels of the bacterium were reduced by two-thirds in participants’ nasal samples.
Also, the probiotic supplement did not disrupt or harm the gut’s normal balance of bacteria — a troubling side effect of antibiotics.
“These results show safety and efficacy of the B. subtilis probiotic in reducing S. aureus human colonization, offering a previously unavailable method to eradicate the main, intestinal reservoir of S. aureus without the considerable dangers of pathogen overgrowth that are associated with systemic oral antibiotic treatment,” write the study authors.
Conclusion
“In conclusion, our findings suggest that B. subtilis probiotic could be used to reduce S. aureus and MRSA colonization prevalence and thus might have clinical potential to lower infection rates, for example in individuals with a history of recurring S. aureus infections or in long-term care facilities, such as nursing homes, with notoriously increased S. aureus colonization and infection risks. Although no known S. aureus decolonization procedure can achieve long-term protection from recolonization, the probiotic strategy, in contrast to any antibiotic-based strategy, offers the possibility for daily and long-term application, because it does not harm the microbiota nor trigger the development of antibiotic resistance. Furthermore, our data provide support for the notion of a dominating role of the intestinal site for S. aureus colonization, suggesting that S. aureus decolonization efforts should generally focus on intestinal rather than, or at least in addition to, nasal colonization.”